Healthcare Reform in Japan; what is the impact for the pharmaceutical industry?
The 2022 Reform of Medical Fees: a quick summary
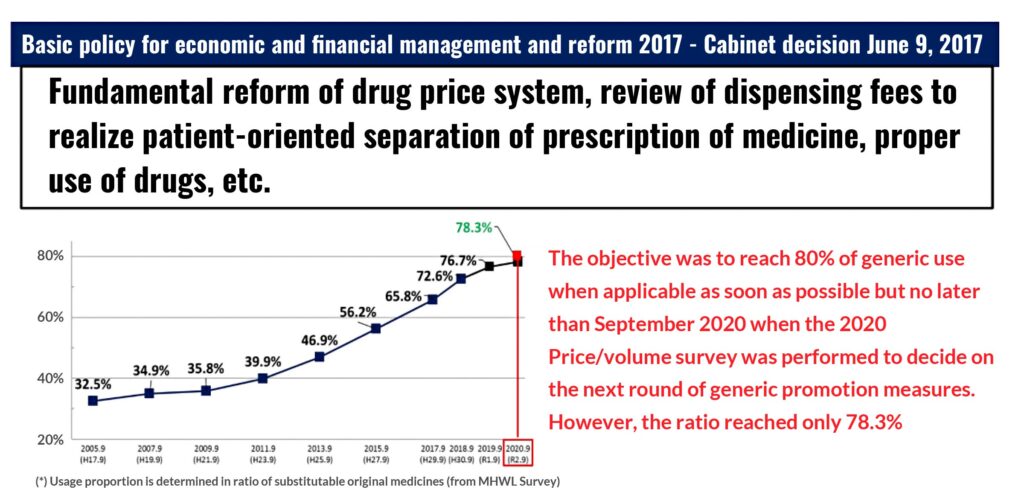
Pursuing a persistent effort over 20 years since the introduction of medical fee points designed to promote the usage of generic drugs in 2002, the Ministry of Health, Labour and Welfare (MHLW) confirmed this time again the promulgation of discrete measures to keep up with the target of higher substitution rate.
The action to aggressively promote the usage of generic medicines really took off from the Reform of 2014 with the definition of quantitative targets, both in terms of absolute numbers and in terms of usage ratio. It was then concretely included in the DPC/PDPS (comprehensive payment system by diagnosis group classification) evaluation system to give a boost to the pro-generic policy sponsored by the MHLW. From the Reform of FY2014, promoting the use of generic drug prescription became part of the strategy to increase medical fees.
The incentive system experienced a new boost in FY2018 Reform when MHLW decided to move the evaluation system from the coefficient class-II to class-I, which resulted in raising the basic score that DPC hospitals were keen to achieve to generate more revenues.
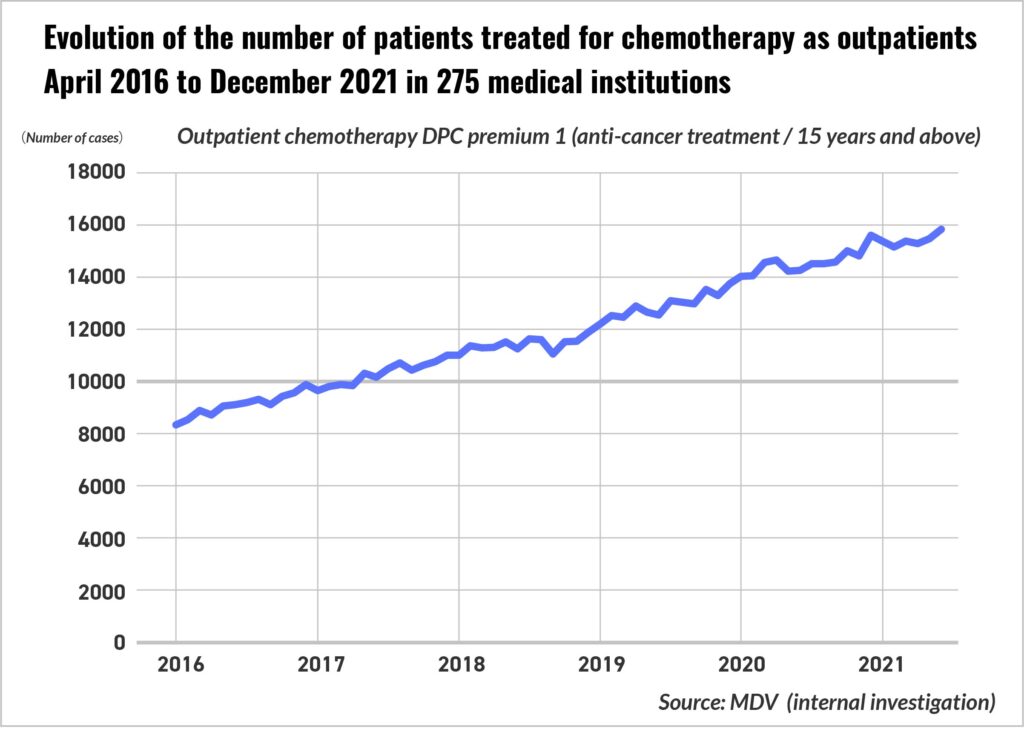
Despite such efforts, the famous target of 80% substitution rate that the government had set in 2017 could not be achieved by September 2020. In July 2021, Central Social Insurance Medical Council, better known as Chuikyo, issued its recommendation for the upcoming 2022 Reform by encouraging a legislation promoting “Outpatient Chemotherapy” that would include a 150-point incentive if biosimilar drugs were to be administered.
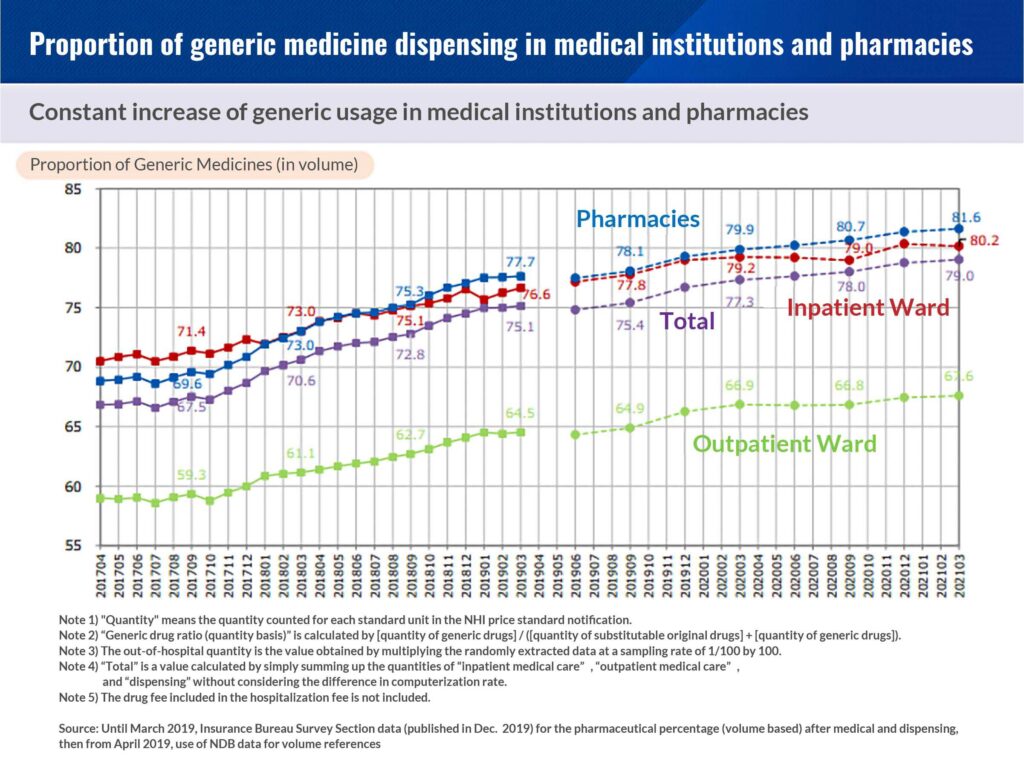
For medical institutions, the addition of the generic drug use system is a new source of profit increase that would come on top of the medical practice just by increasing the usage rate of the generic drug based on the previous Reform of FY2020, when an addition of 47 points or more was granted for the first day of hospitalization or the DPC function evaluation coefficient 0.0014 that grants at least 5 points to prescription fee for outpatients.
It is natural for a manager to think that if a net profit can be secured by increasing the usage rate of generic drugs without considering the drug price margin, it should represent a stable financial resource. However, MHLW goal is not to promote the usage of generic as such, but the replacement of original medicine whenever the option is available when the patent or exclusivity expired. With the successive revisions of the medical fees structure since FY2014, pushing for the higher use of generic higher in the hospital management priorities but it is clear that the Reform of FY2022, by setting for the fourth time a new threshold for generic usage rate, delivers a strong message to hospitals. When a sailing boat catches the tailwind, it is common to think that it is hard to change direction. For hospitals, whatever the sea might turn to be, the wind clearly blows in the direction of proactive and committed substitution.
For further reference; MHLW – December 18, 2021 Chuikyo appendix (part 8)
https://www.mhlw.go.jp/content/12404000/000863578.pdf
Certified nurse, specific training and cancer treatment
In the FY2022 revision of medical fees, under the theme of task shifting / task sharing, the existence of professionally educated nurses in the clinical setting has finally come to light.
The certified nurse system was established in 1995 for the purpose of training highly specialized nurses, and the revised Public Health Nurse, Midwife and Nurse Law (改正保助看法) was enforced in October 2015, describing specifically the actions that nurses can carry out. A training system (specific action training) was established. In FY2020, specialization training has been included in the curriculum for certified nurse education by the Japanese Nursing Association.
However, for nurses who obtained certification before 2020, it was only stated in the facility standards for medical fees that they had received specialized training related to a specific therapeutic area, but in the FY2022 revision, “Specialization Training” bonus is proposed. Hospitals would receive credits to actively promote the “specialization training” in the facility standard by calculating additional points when employing such skilled nurses related to medical care team, which is labeled under the initiative of “promotion to optimize human resources”.

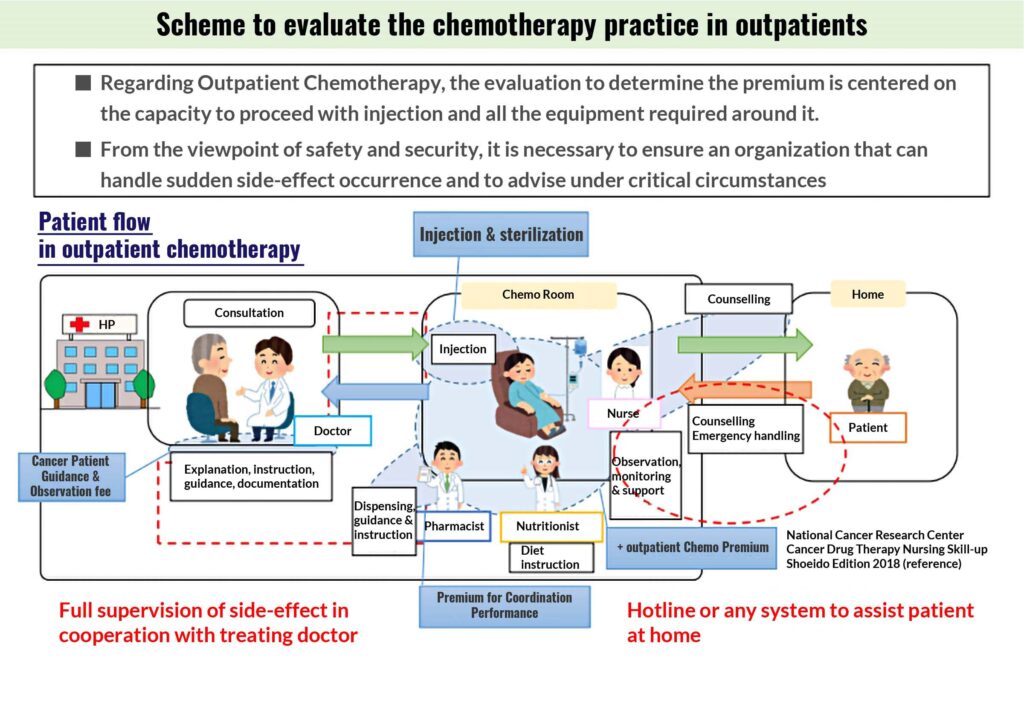
Under these circumstances, “cancer chemotherapy nursing”, one of the pioneer program in the nursing certification system, was changed to “cancer drug therapy nursing”, and a new stage of activity was created. This new stage is the “outpatient tumor chemotherapy fee”.
Regarding the conventional “outpatient chemotherapy premium”, the role of co-medics such as nurses, pharmacists, and registered dietitians has been highlighted from the background so far, but in the FY2020 revision, it has been raised to a top priority issue in the discussion of Chuikyo.
From Chuikyo Assembly (2020, October 22) – 中医協 総―1
In the recommendations issued by Chuikyo, the points added in relation to the involvement of pharmacists and registered dietitians are eye-catching, but when carrying out outpatient chemotherapy, “cancer specialist nurses” who are always close to the patient who receives treatment directly facing the patient are most likely to take a pivotal role in the handling of cancer therapy over the coming years.
References:
Ministry of Health, Labour & Welfare, October 22, 2021, Chuikyo General Assembly Appendix part 2
https://www.mhlw.go.jp/content/12404000/000846288.pdf
Ministry of Health, Labour & Welfare, February 9, 2022, Chuikyo General Assembly Regarding each item of the Reform
https://www.mhlw.go.jp/content/12404000/000894869.pdf
[kengo_tabnaka2]
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
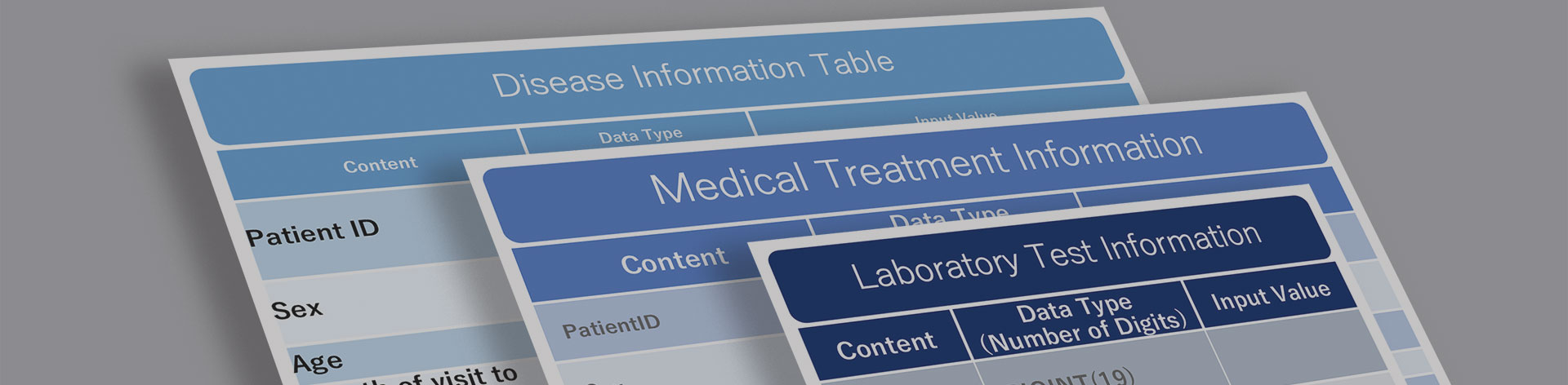
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





