Insurance Database for Claims: Cutting Healthcare Costs
Contents
- Key Takeaways
- The Role of Insurance Data in Healthcare Cost Management
- Using Claims Data For Preventative Care and Early Intervention
- How Claims Data Helps Improve Medical Device Design and Patient Safety
- Forecasting Healthcare Needs with Claims Data
- Collaborating with Insurers to Close Gaps in Medical Care
- How MDV’s Claims Data is Shaping the Future of Healthcare
- Frequently Asked Questions
Key Takeaway
An insurance database for claims is important for improving healthcare cost management, driving preventative care, and boosting the innovation of new medical devices. Claims data helps healthcare providers reduce costs and prevent chronic conditions by identifying early risks. This data also guides manufacturers in designing more effective medical devices. Collaboration between insurers and manufacturers ensures that gaps in care are addressed, leading to better patient outcomes and a more efficient healthcare system.
Using an insurance database for claims analysis provides more than just insights for research and development. It can also provide a wealth of real-world data that can be used to improve healthcare outcomes, optimize preventative care, and enhance cost efficiency. By analyzing patient treatment patterns, diagnoses, and healthcare use statistics, insurers and medical device manufacturers can identify the different trends that highlight gaps in care, pinpoint at-risk populations, and develop custom interventions that can help prevent costly complications down the road.
Collaboration between insurers and manufacturers creates a mutually beneficial approach. Insurers have the advantage of reducing costs by preventing unnecessary treatments and hospitalizations, while manufacturers can gain valuable insights into how their devices perform in real-world settings. This approach leads to improved patient outcomes, better resource allocation, and much more effective medical innovations. The insurance database for claims is an important tool that plays a big role in benefiting both patients and healthcare providers alike.
The Role of Insurance Data in Healthcare Cost Management
The use of an insurance database for claims is becoming increasingly more important in addressing the rising costs of healthcare. As healthcare costs continue to soar, using claims data gives healthcare providers and insurers the ability to manage their expenses by identifying the different patterns in the data that can help reduce any unnecessary hospitalizations and emergency care. By analyzing this data, providers can pinpoint opportunities for early interventions and preventative care, which in the end will lead to significant cost savings.
By using an insurance database for claims, both healthcare professionals and insurers can identify high-cost patients before their health declines, allowing for proactive care that avoids the more expensive, reactive treatments. This approach is especially valuable in managing chronic diseases, where early detection and targeted interventions can prevent complications that are much more difficult to treat.
Plus, the data that becomes available from claims databases allows insurers to adjust their policies based on real-world evidence. This can include promoting cost-effective treatments or discouraging procedures that may be unnecessary. When combined with predictive analytics, claims data is a very powerful tool for forecasting future healthcare costs and resource use. For example, by analyzing historical claims, insurers can anticipate which patients may require more expensive care and implement preventive measures to lower costs.
In addition to this, claims data can highlight trends in patient care that offer actionable insights for both insurers and healthcare providers. These different trends can range from common treatment paths for specific conditions to identifying high-utilization services that significantly contribute to rising healthcare costs.
Using Claims Data For Preventative Care and Early Intervention
An insurance database for claims plays a very important role in preventing the escalation of chronic diseases. It does so by identifying at-risk patients much earlier on. By analyzing claims data, insurers and manufacturers can collaborate with one another to detect patterns that signal the onset of conditions like diabetes, hypertension, or heart disease before they worsen. This collaboration can lead to targeted interventions that help prevent costly hospitalizations and long-term complications.
For example, a clinical study using the Korean National Health Insurance Service (NHIS) database proved how claims data can show specific risk factors for chronic conditions such as rheumatoid arthritis. By analyzing the available patient data, researchers were able to track early symptoms, monitor adherence to treatment, and predict which patients were most likely to experience disease progression. This level of insight, taken from real-world data, allows for better early interventions, significantly reducing the overall burden of the disease and improving long-term patient outcomes.
Plus, analyzing an insurance database for claims can reveal trends in how healthcare is being used. For instance, claims data can show which patients frequently visit emergency rooms for conditions that could be better managed through primary care. Having this information gives insurers a better ability to recommend preventative treatments.
Preventative care strategies driven by claims data have the potential to address high-cost patients early on, which goes a long way toward helping healthcare systems deliver more affordable care to their patients. By identifying these patients through patterns in their healthcare usage and the outcomes of their care, insurers and manufacturers can implement early intervention programs that reduce long-term treatment costs and therefore improve the health of their patients.
How Claims Data Helps Improve Medical Device Design and Patient Safety
The use of an insurance database for claims is continuing to prove to be an invaluable tool for medical device manufacturers that want to improve the design of their products. By analyzing real-world claims data, manufacturers can identify patterns of device usage, complications, and patient feedback that may not always be clearly visible in the clinical trials that they perform. This allows for the development of safer, more user-friendly devices that better meet the needs of their patients.
For example, in a study on the use of real-world evidence (RWE), claims data helped identify that certain medical devices, such as heart valves, showed unanticipated complications in real-world use. These specific findings ultimately led to adjustments in the design of these devices, improving their overall safety profile and significantly reducing the chance of any adverse events. This type of data helps manufacturers stay informed about how their devices perform in everyday settings, outside of controlled clinical trials. The study on real-world evidence emphasizes that data from claims databases, such as Medicare in the United States, and other insurance providers, offers a broader range of patient data, which includes diverse demographics and real-world conditions, helping manufacturers to spot issues that they may not be able to see otherwise.
A practical case of this is the FDA’s use of post-market claims data to evaluate the safety of the Thoratec Heartmate II left ventricular assist device. By monitoring claims and reports of thrombosis (blood clotting), device manufacturers were able to identify a significant increase in adverse events. This led to a device redesign, which then resulted in reduced incidents of thrombosis and improved the long-term outcomes for patients relying on this life-saving technology.
Claims data doesn’t just help in identifying issues—it also contributes to cost efficiency. By using data from an insurance database for claims, manufacturers can predict which patient groups are at higher risk of complications, giving them the opportunity to improve device designs that reduce the need for long-term care and the possibility of additional procedures. This results in substantial cost savings for both healthcare providers and patients.
Forecasting Healthcare Needs with Claims Data
Using an insurance database for claims for predictive analytics has become a must-have tool for healthcare providers and insurers in order to forecast future healthcare needs. By analyzing historical claims data, healthcare organizations can identify trends, anticipate future healthcare demands, and make more informed decisions.
One of the biggest benefits of predictive analytics is the ability to assess long-term patient care needs. For example, claims data can identify patients who are at higher risk for chronic conditions such as diabetes or heart disease. By detecting early warning signs through data analysis, healthcare providers can intervene earlier, offering preventative care and treatments that reduce the need for costly emergency care or hospitalizations. This leads to better patient outcomes while also helping to control healthcare spending.
The predictive power of claims data also extends to planning for larger public health needs. During the COVID-19 pandemic, for example, predictive models based on claims data were used to forecast the demand for ventilators, hospital beds, and other essential medical resources. This allowed healthcare systems to better prepare, ensuring that they had the necessary supplies and equipment to handle the surges in patient numbers. In the future, predictive analytics could play an even greater role in planning for pandemics or other public health emergencies.
In addition to public health preparedness, claims data also helps healthcare providers and insurers better budget for long-term care needs. Predictive modeling based on insurance database for claims allows organizations to estimate the future demand for specific medical devices or treatments. For example, as claims data reveals the increasing prevalence of aging-related conditions such as arthritis, healthcare providers can anticipate a growing demand for assistive devices like knee or hip implants. This ensures that manufacturers can produce enough devices to meet future demand, while healthcare providers can allocate the necessary budget for these treatments.
By relying on insurance database for claims, healthcare systems and insurers can create more accurate budgets, avoid costly surprises down the road, and ensure that they are prepared for both everyday healthcare needs and larger-scale events.
Collaborating with Insurers to Close Gaps in Medical Care
Collaboration between medical device manufacturers and insurance companies is playing an increasingly important role in advancing innovation in healthcare. By working together, both parties can take advantage of the valuable insights that are provided by an insurance database for claims to drive the development of next-generation medical devices. This partnership allows manufacturers to align their product development with real-world healthcare needs, ensuring that new devices address the gaps in care that claims data reveal.
For instance, claims data can highlight areas where current treatments or devices are falling short. Whether it’s identifying unmet needs in chronic disease management or revealing patterns in patient non-compliance with certain devices, the insurance database for claims offers a data-driven foundation for manufacturers to create more effective and user-friendly products. This data allows companies to target specific issues, resulting in devices that better serve their patients while also striving to reduce healthcare costs.
Plus, this collaboration helps to grow the creation of innovative business models, such as shared risk agreements. In these models, manufacturers and insurers work together, sharing both the data and the responsibility for patient outcomes. By using this arrangement, insurers provide manufacturers with access to detailed claims data, which is then used to guide product design and improvements. In return, manufacturers agree to link the success of their devices to actual patient outcomes, aligning their incentives with the broader goals of healthcare improvement.
By partnering with insurers, manufacturers can stay ahead in the market by developing devices that meet both patient needs and insurer requirements. This collaborative approach drives innovation and also ensures that new devices are integrated seamlessly into the healthcare system, improving outcomes for everyone involved.
How MDV’s Claims Data is Shaping the Future of Healthcare
Using the power of an insurance database for claims like MDV in Japan offers healthcare providers and manufacturers valuable insights into patient care trends, chronic disease management, and opportunities for medical innovation. With data covering over 45 million patients from 480 hospitals, MDV’s claims data helps inform strategic decisions that lead to better outcomes, reduced healthcare costs, and the development of next-generation medical devices. As the healthcare industry continues to evolve, embracing data-driven approaches such as these can significantly enhance patient care and boost operational efficiency.
If you’re looking to explore how claims data can support your organization’s healthcare solutions, reach out to learn more about how MDV data can transform your approach.
Frequently Asked Questions
What is a claims database?
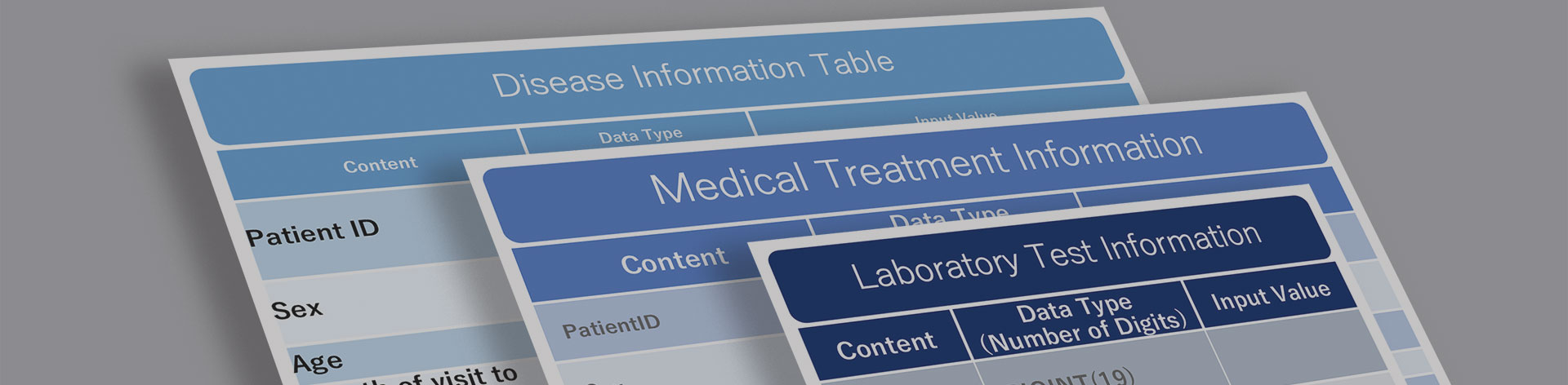
A claims database is a collection of detailed records about patient treatments, diagnoses, and healthcare services that are used for insurance and billing purposes. These databases capture critical information on the care patients receive and are vital for both healthcare providers and insurers in managing both care and costs.
What is an insurance database for claims?
An insurance database for claims is a centralized system that stores and organizes insurance claims data. It provides insights into patient care, medical treatments, and healthcare trends. This data helps insurers, healthcare providers, and medical device manufacturers to make informed decisions about patient care, improve service delivery, and identify areas for innovation.
What database do insurance companies use?
Insurance companies use various types of databases depending on the country and healthcare system. For example, in Japan, the MDV database is widely used, covering more than 45 million patients from 480 hospitals. These databases provide critical information for analyzing healthcare patterns and improving patient outcomes.
How does an insurance database for claims help reduce healthcare costs?
By analyzing data from an insurance database for claims, healthcare providers and insurers can identify patterns that drive up costs, such as unnecessary hospital readmissions or late-stage chronic condition interventions. Early identification of at-risk patients through claims data can lead to preventative care measures, reducing the overall costs of long-term care.
How does claims data drive medical innovation?
Medical device manufacturers use claims data to understand real-world usage of their products. Insights from these datasets allow manufacturers to refine the design, functionality, and safety of medical devices, resulting in innovations that improve patient outcomes, increase compliance, and reduce the need for additional treatments or interventions.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





