7th Release – Medical Expenditures and Hospitals
Part #4: Drug Management and Dispensing Pharmacy
Note: The opinion of the author expressed in the article does not represent any official opinion or position of Medical Data Vision regarding the 2022 Reform of the Medical Fees. The series of article is designed to provide insight and matter to discuss the healthcare environment among various stakeholders. Thanks for your understanding.
Number of pharmacists allocated
“Article 19(2) (i) of the Medical Care Act (Pharmacist): the sum of the number obtained by dividing the number of patients hospitalized in hospital rooms with psychiatric beds or long-term care beds by 150, the number obtained by dividing the number of patients hospitalized in hospital rooms other than those with psychiatric beds or long-term care beds by 70, and the number obtained by dividing the number of prescriptions handled for outpatients by 75.”
In 1998, when the Winter Olympics were held in Nagano Prefecture, Japan, standard number of hospital pharmacists was reconsidered in the third revision of the Medical Service Act, and the new standard number of hospital pharmacists was stipulated in the Enforcement Regulations of the Medical Service Act.
At that time, the number of pharmacists assigned to dispensing pharmacies was also set at “one pharmacist for every 40 prescriptions.” From this time on, the staffing standards for dispensing pharmacies became more generous than those in hospitals.
Since 1989, MHLW has instructed 37 model national hospitals at that time to actively issue out-of-hospital prescriptions (complete division of duties, out-of-hospital prescription delivery rate of over 70%), and in fiscal 1997, the rate exceeded 35% (MHLW press release, “Out-of-hospital Prescription Delivery at Model National Hospitals, FY1995” https://www.mhlw.go.jp/www1/houdou/0807/0730-1.html ), and in fiscal 2020, the total rate of out-of-hospital prescription by health care insurance was 77.3% (Summary of Statistics of Social Medical Practice, 2020 https://www.mhlw.go.jp/toukei/saikin/hw/sinryo/tyosa20/dl/gaikyou2020.pdf ).
On the other hand, as for the work of pharmacists involved in inpatient care, the medical fee that could be calculated for explaining drugs to patients as an inpatient dispensing technique fee was changed to a “drug instruction and management fee” in the 1994 revision of medical fees, and a major revision was made to allow a maximum of 600 points per patient per month. In 1998, the fee was further increased to a maximum of 1,060 points per patient per month.
Drug Administration Instruction and Dispensing Pharmacy
From the perspective of hospital management, the minimum number of employees required by the Medical Services Act must be met, even if it is not possible to employ a sufficient number of people. In other words, the ideal system should be one that, increasing medical revenue while adhering to minimum staffing standards. The promotion of out-of-hospital prescription and the separation of dispensary from medical practice has been loudly announced, the number of points has been increased accordingly, and if the revenue from instruction and management fees, which have no source of funds, is greater than the revenue from an unstable marginal profit on drug prices in a sense, it is impossible not to benefit from this.
Hospital pharmacists have shifted their duties to providing drug administration instruction to inpatients, and the labor shortage led to a shift to prescribing outside of the hospital for outpatients.
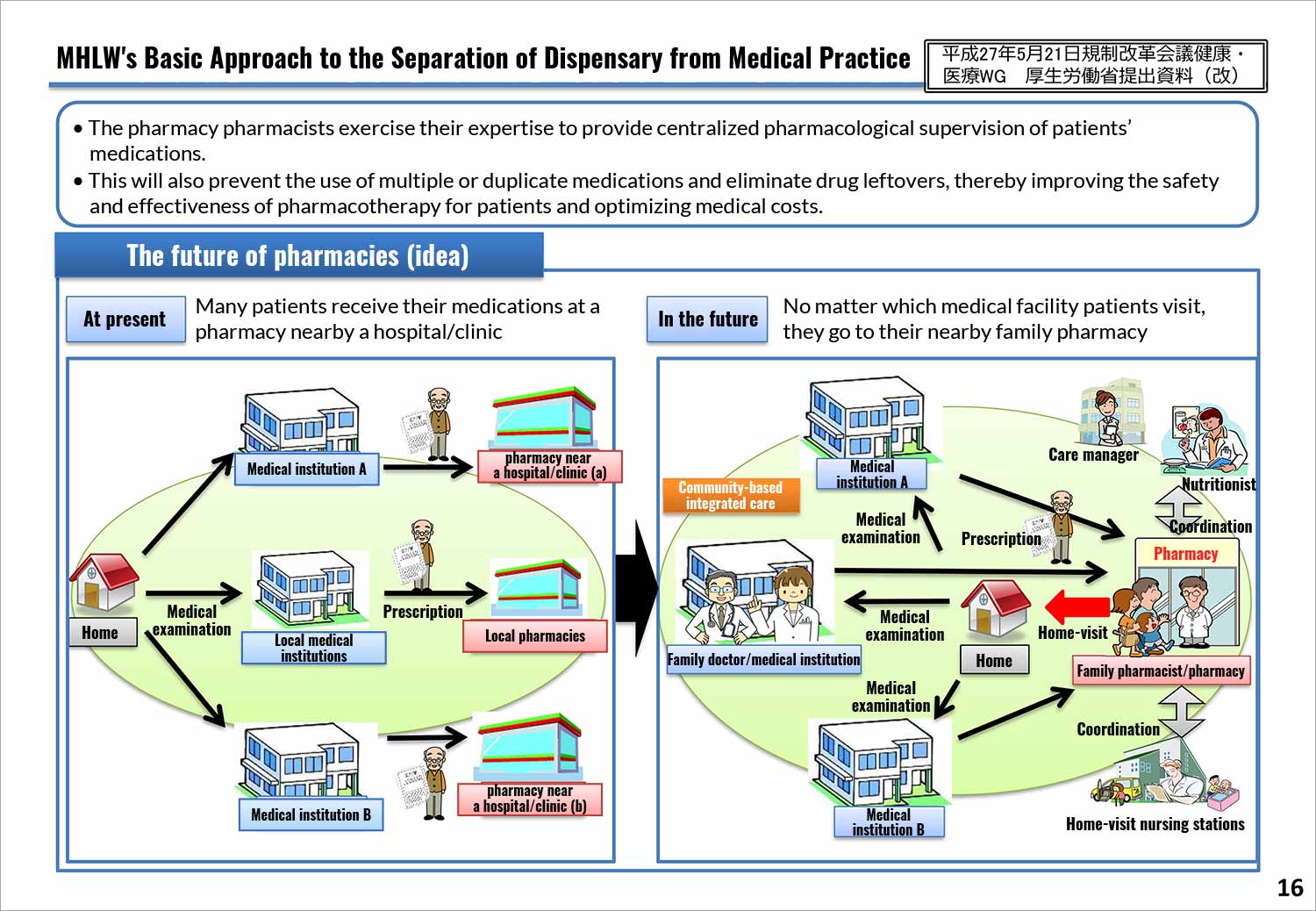
As a result, pharmacies have invaded the city streets, but in order to protect the fairness of the location environment and purchase prices, measures had to be taken to ensure that profits are not biased in favor of specific businesses entity, such as reducing the dispensing fee for pharmacies near a hospital/clinic (specific dispensing basic fee) and setting a base dispensing fee for the same group of dispensing pharmacies (base dispensing fee 3), etc.
In the 2022 revision of the medical service fee system, the restrictions that had been imposed only on dispensing pharmacies are now also imposed on medical institutions that prescribe drugs. For example, the “additional fee for acute phase enhancement system” cannot be calculated for hospitals that provide highly acute care if they have an on-site pharmacy.
In addition to the negative revision of drug prices, the medical service fee system for dispensing pharmacy services appears at first glance to have become tougher with a strong trend toward point reductions. However, taking another look at the contents of the 2022 medical service fee revision, the “goods to people” policy, which the Central Social Insurance Medical Council has set as a theme for the work of pharmacists, is strongly evident, and pharmacy pharmacists in dispensing pharmacies have received generous points for their work in guidance and drug management.
The implementation of refill prescriptions began, and high expectations were placed on family pharmacies with regard to measures against polypharmacy.
The separation of dispensary from medical practice, which began with the issuance of out-of-hospital prescription, has brought about an era in which both parties work together to treat patients by figuring out how to maximize the use of the resources that both parties have.
October 22, 2021 (Friday) 492nd General Meeting of the Central Social Insurance Medical Council (Prescription Part 2)
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





