7th Release – Medical Expenditures and Hospitals
Part #6: End-of-life care
Note: The opinion of the author expressed in the article does not represent any official opinion or position of Medical Data Vision regarding the 2022 Reform of the Medical Fees. The series of article is designed to provide insight and matter to discuss the healthcare environment among various stakeholders. Thanks for your understanding.
Trending in the number of patients
[Hospitals: 938,130 persons (68.3%), Clinics: 21,455 persons (1.6%), Nursing care hospitals, elderly healthcare facilities, etc.; 45,606 persons (3.3%), Senior citizens’ home: 125,722 persons (9.2%), At home: 216,103 persons (15.7%), Others: 25,738 persons (1.9%)]
These figures are from the Vital Statistics 2020, a breakdown of 1,372,755 deaths by place of death in 2020. [Figure 1]
The number of deaths in medical institutions, including clinics, increased rapidly after 1975, reaching the 70% threshold in 1990, and at one time, more than 80% of deaths occurred in medical institutions, but in 2020, the figure dropped to 70%.
Meanwhile, the number of deaths is expected to continue to rise until 2040, reaching an estimated 1.66 million in that year. [Figure 2]
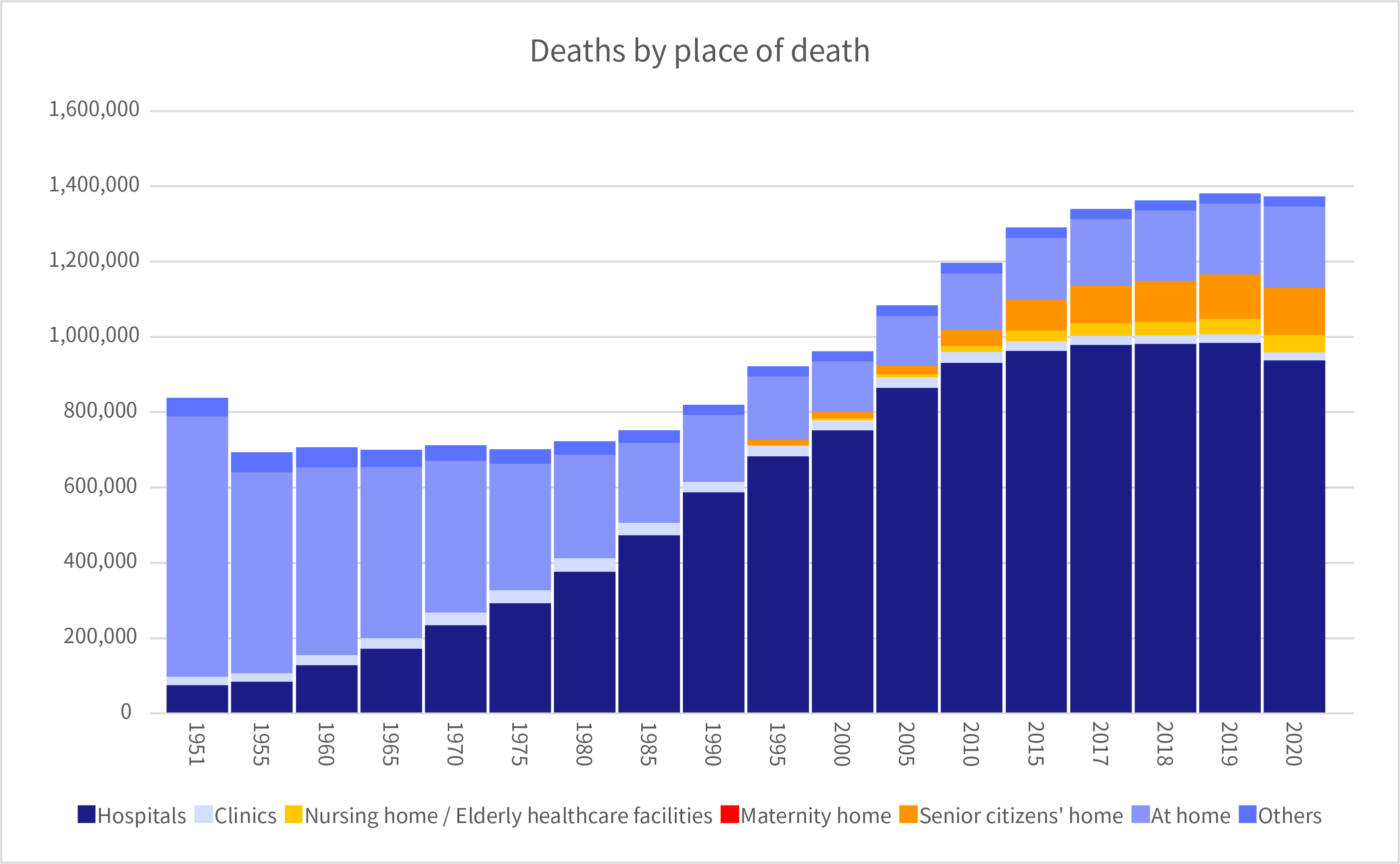
[Figure 1] https://www.mhlw.go.jp/toukei/youran/indexyk_1_2.html
Compiled from the Handbook of Health and Welfare Statistics 2021, Part 1, Population and households, Chapter 2, Vital Statistics.
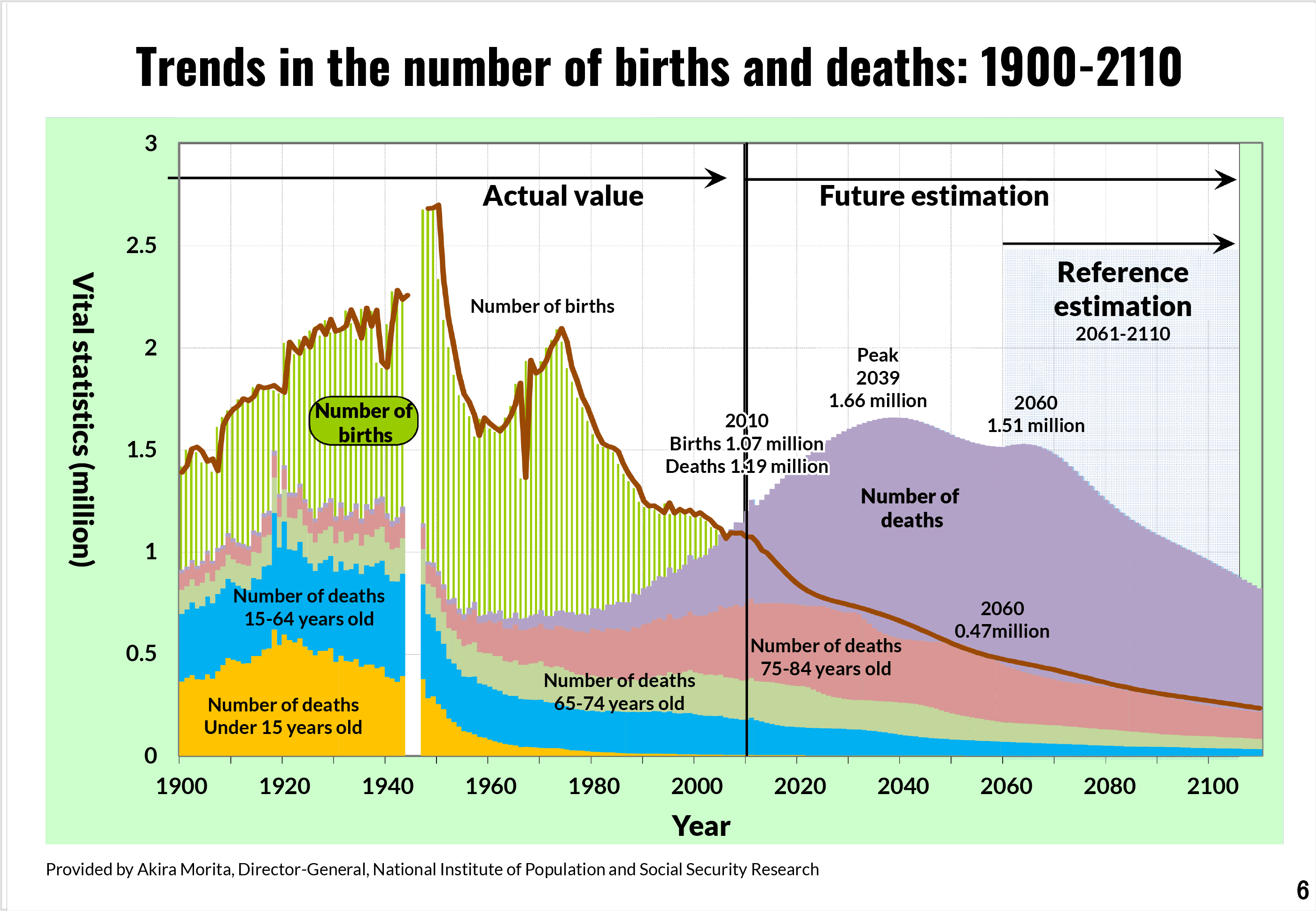
[Figure 2] https://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000167844.pdf
Abstract from the Central Social Insurance Medical Council General Meeting in December 14, 2016 “Current Situation and Issues Surrounding Medical Care and Elderly Care, etc.”
In terms of the number of beds in operation, as indicated by the number of hospital beds required in 2025 in the medical community concept, both highly acute-phase and acute-phase beds and chronic-phase beds will decrease.
This means that at the current rate of places of death, approximately 1.16 million people will die in medical facilities, but is there really enough capacity to accommodate this number of deaths?
Who will be responsible for end-of-life care?
In July 1987, the “Investigative Commission on the State of Medical Care in the Last Stage of Life” was formed and a survey of public and medical professionals’ awareness has been started. In 2007, the study group published “Guidelines for the Decision-Making Process for Medical Care and Care in the Final Stage of Life,” a revised version of which was released in 2018, specifying what patients and their families, as well as medical professionals, should address with regard to end-of-life care.
In its 2017 report, that the investigative commission revealed that the majority of the population prefers to be cared for at home with regard to where they would like to spend their time in the last stage of life.
Results of 2017 Awareness Survey Report on Medical Care in the Last Phase of Life (Final Version) I-8 Preferences regarding where to spend time in various end of life situations (1) Places where you would like to receive medical care and treatment. [Case 1]
https://www.mhlw.go.jp/file/05-Shingikai-10801000-Iseikyoku-Soumuka/0000200749.pdf
However, under the current medical care provision system, the reality is that most of these patients spend their final days in hospitals (see above).
On the other hand, the medical community concept calls for the enhancement of the at-home medical care system, including the enhancement of terminal care, as a measure to realize the future medical care system.
In addition, in the 2022 revision of medical fees, an additional fee for remote diagnosis of death was newly established as one of the medical procedures using information and communication devices, as a medical fee point that allows death confirmation in the presence of a visiting nurse.
A discussion on who will be responsible for providing end-of-life care is needed, along with the direction that the hospital should take in promoting regional cooperation.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE

In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





