7th Release – Medical Expenditures and Hospitals
Part #5: Revision of Medical Fees: What was Required of Medical Institutions?
Note: The opinion of the author expressed in the article does not represent any official opinion or position of Medical Data Vision regarding the 2022 Reform of the Medical Fees. The series of article is designed to provide insight and matter to discuss the healthcare environment among various stakeholders. Thanks for your understanding.
Additional Fee for phase Enhancement System
A little more than seven months have passed since the 2022 revision of medical fees.
Most items of the transitional measures established in correlation with the revisions have now expired, and the effects of the revisions are starting to become apparent.
During the transitional period, some facilities may have adapted their intra-hospital environment to the new standards, while others may have reevaluated their hospital systems and decided to calculate medical fees that match the systems with their own hospitals.
Amidst such situation, the number of facilities that had notified “additional fee for acute phase enhancement system,” which was a sensation among acute-care hospitals in the 2022 revision of medical fees, to the Health and Welfare Bureau was 157 as of September 1, 2022 (National Bureau of Health and Welfare notification status, according to MDV’s survey).
In addition, taking into consideration the fact that 391 facilities had notified “additional fee for comprehensive hospitalization system” as of May 2021 but 255 facilities had notified it as of September 1, 2022 (National Bureau of Health and Welfare notification status, according to MDV’s survey), it can be inferred that facilities that have satisfied the facility criteria for “additional fee for acute phase enhancement system” for advanced or acute phases could switch to “additional fee for acute phase enhancement system” with almost no barriers.
Originally, the name and facility standards for the “additional fee for comprehensive admission system” were revised in 2010 from the former “additional fee for medical management at the time of admission” in order to evaluate general hospitals that provide more advanced medical care, and the definition of the calculation was revised in FY2022 as well.
At first glance, many of the facility standards required for registration of the “additional fee for acute-phase enhancement system” and the “additional fee for comprehensive admission system” are very similar, but the “additional fee for acute-phase enhancement system” is defined in such a way as to avoid uneven distribution of large hospitals by applying a detailed number of performance based on the number of sickbeds, and it seems that the performance as a highly acute and acute phase medical institutions is finally being properly assessed.
Recovery / Chronic Phase
Now, let’s shift the attention to the recovery and chronic phase.
Although there is a two-year transitional period for admission charges 5 and 6, admission charges for recovery-phase rehabilitation wards will be abolished (admission charges 6 will be abolished by March 2023)*, and the calculation criteria for basic admission charges for long-term care wards have also been tightened with the introduction of the measurement of functional independence method (FIM) as a requirement.
* Overview of 2022 Revision of Medical Fee (Full Version)
https://www.mhlw.go.jp/content/12400000/000960258.pdf (*p.57)
Looking at the situation only in terms of notification results, the number of facilities that notified admission charges for recovery phase rehabilitation wards increased from 1,531 as of May 2021 to 1,553 as of September 1, 2022, while the number of facilities that notified basic admission charges for long-term care wards decreased from 2,977 as of May 2021 to 2,922 as of September 1, 2022. In addition, the number of facilities notifying basic admission charges for bedside clinics (including facilities with basic admission charges for long-term care bed for bedside clinics) also decreased significantly, from 4,932 to 4,728.
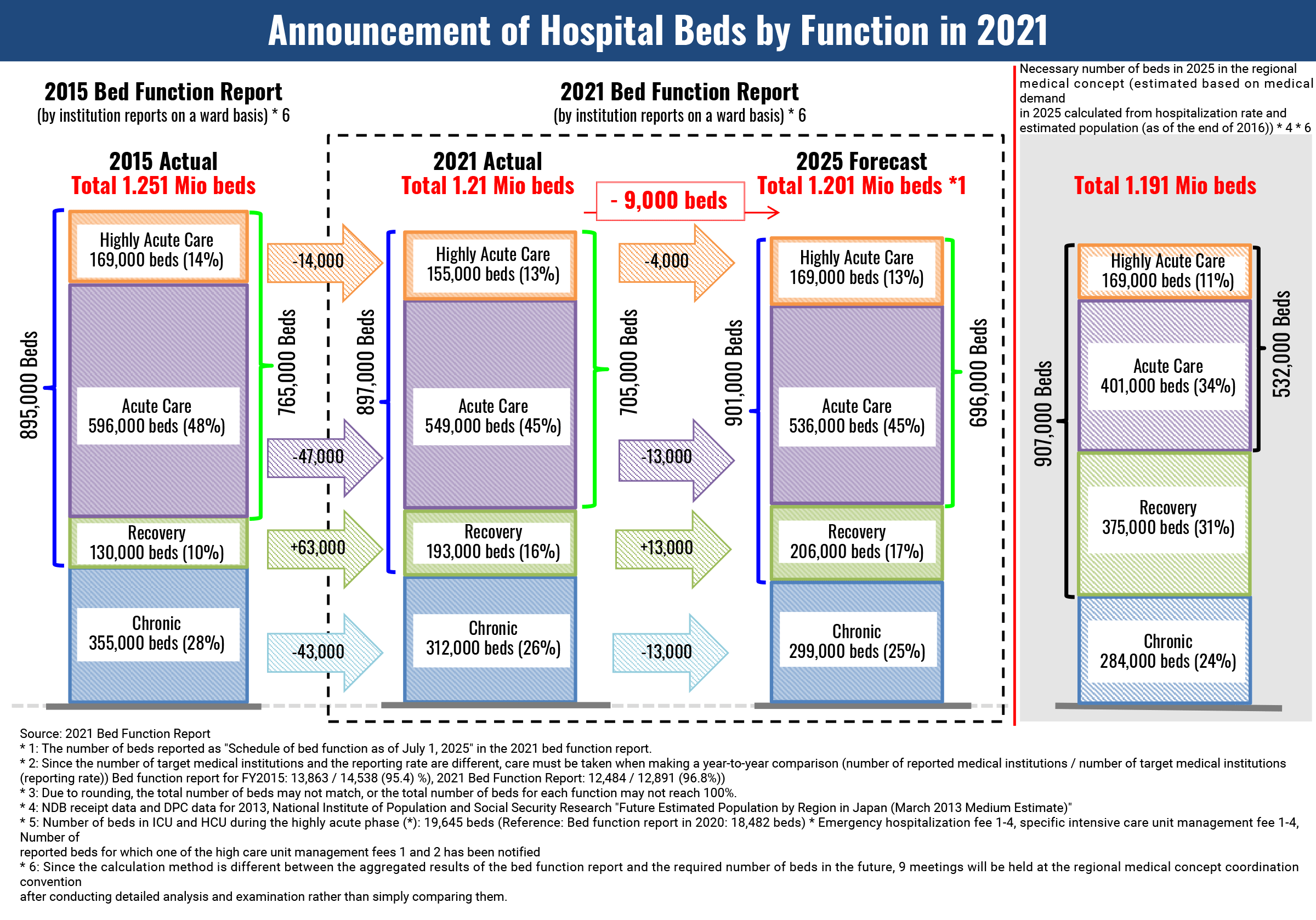
From a micro perspective, this is the result of each hospital’s management efforts, but from a macro perspective, this phenomenon is consistent with the progress envisioned by the Ministry of Health, Labour and Welfare (MHLW) in its regional medical care vision in 2025.
Working Group on the 5th Community Healthcare Initiative and Doctor Recruitment Plan “Regarding the implementation of the bed function report in 2022”
On September 26, 2019, the same month as the inauguration of the fourth Abe administration, MHLW compiled specific measures and methods for re-verification and released data on individual medical performance results of public medical institutions, etc., and has positioned 424 hospitals among those facilities that “require discussion, especially with regard to restructuring and integration.”
This announcement caused quite a stir at the time.
Currently, each prefecture is preparing a regional medical plan, and the status of the discussion is to be made public periodically (the latest announcement was made at the end of September, 2022, on each prefecture’s homepage, etc.).
Medical facilities, especially public ones, must squarely face the regional medical care vision.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE

In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





