Hospital Bed Functional Differentiation in Japan: Impact on Healthcare, Pharma, and Patients
In Japan, the concept of hospital bed functional differentiation refers to the reorganization of existing hospital beds, currently divided into general and long-term care beds, into four categories: advanced acute care, acute care, recovery, and chronic care.
This initiative is part of Japan’s healthcare reform in response to the country’s rapidly aging population. By 2025, the entire baby-boomer generation will be over 75, raising concerns of nationwide bed shortages. The reform is designed to optimize medical resources, improve efficiency, and ensure patients receive care suited to their condition.
This article provides an overview of the reform and its implications for healthcare services, pharmaceutical companies, and patients in Japan, highlighting the Japanese hospital system.
What is Hospital Bed Functional Differentiation?
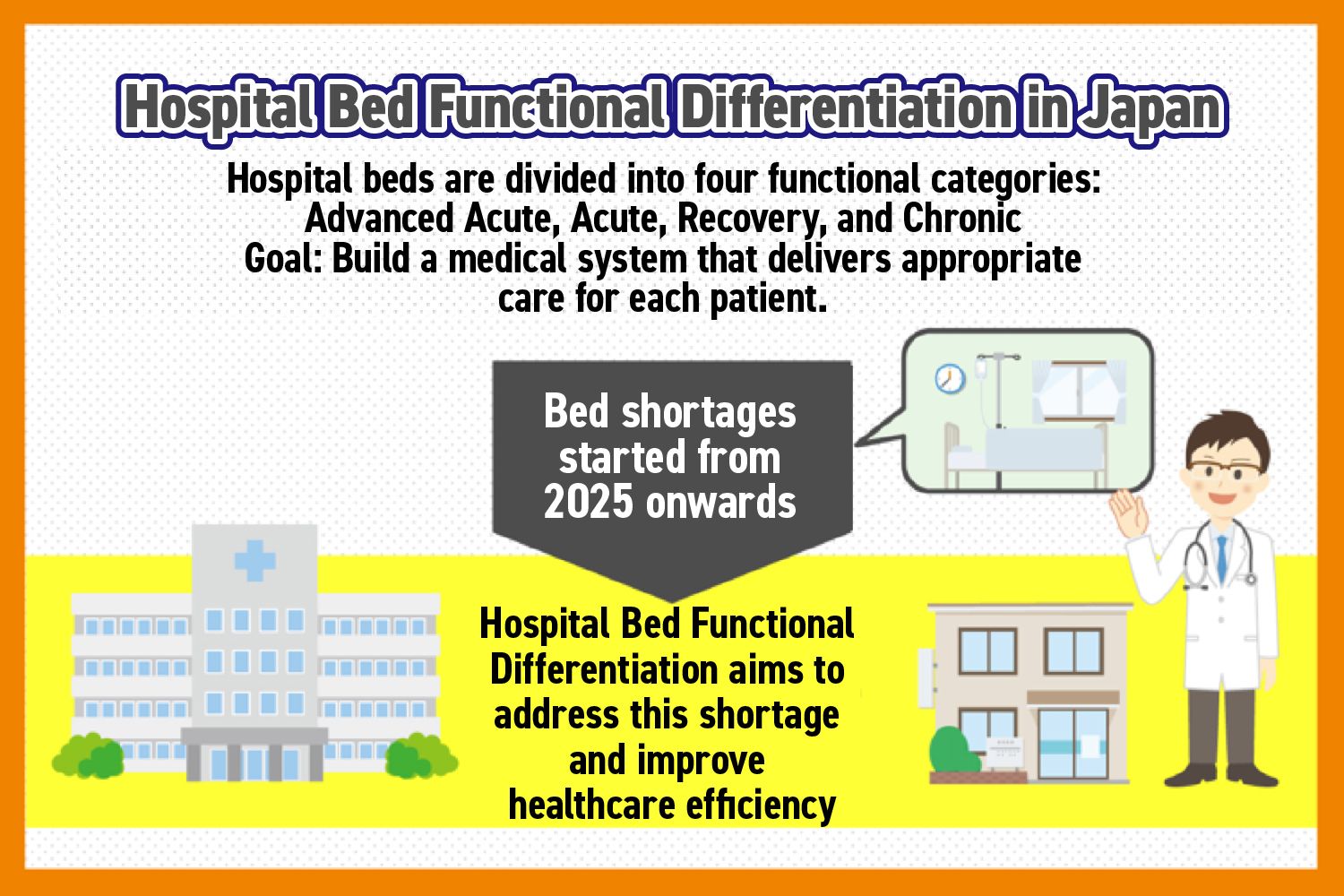
Hospital bed functional differentiation in Japan is a healthcare initiative designed to ensure patients receive quality medical care tailored to their condition by categorizing hospital beds based on function and fostering collaboration between facilities.
Hospital beds were traditionally divided into general and long-term care categories, with certain regions experiencing shortages relative to demand. To address this, the government introduced a plan to reorganize beds into four functional categories: advanced acute care, acute care, recovery care, and chronic care. The goal was to establish a seamless system enabling patients to access appropriate services as needed, spanning from medical care to nursing care.*
As of 2025, most hospitals in Japan have implemented this classification, although some regional differences remain.The Ministry of Health, Labour and Welfare (MHLW) continues to monitor outcomes and adjust policies to ensure balanced distribution and smooth patient transitions.
* Reference: Ministry of Health, Labour and Welfare. Regarding Regional Healthcare Plans, p. 4–6.
https://www.mhlw.go.jp/file/04-Houdouhappyou-10904750-Kenkoukyoku-Gantaisakukenkouzoushinka/0000094397.pdf (accessed November 8th, 2023)
1.Background of Hospital Bed Functional Differentiation
The push for hospital bed functional differentiation arises from the historic imbalance in bed distribution, with an overconcentration of general beds. Because priority is typically given to patients requiring emergency admission, there has long been a shortage of beds for recovery and chronic care patients who need extended treatment or stable nursing care environments.
By 2025, Japan’s baby boomer generation (dankai sedai) all reached the age of 75 or older, further intensifying concerns about hospital bed shortages.*This reform is a key part of Japan’s strategy to modernize the hospital system and ensure sustainable care for an aging population. In response, the government launched the Hospital Bed Function Reporting System in 2014 to collect data and guide redistribution of beds. This reporting system continues to play a central role in tracking progress and identifying areas where functional differentiation remains incomplete.*
* Reference: Ministry of Health, Labour and Welfare. Regarding Regional Healthcare Plans, p. 4–5.
https://www.mhlw.go.jp/file/04-Houdouhappyou-10904750-Kenkoukyoku-Gantaisakukenkouzoushinka/0000094397.pdf (accessed November 8th, 2023)
2. Purpose of functional differentiation
The main objective is to secure sufficient and appropriate bed numbers across the care continuum. Advanced acute care is concentrated in highly specialized hospitals, while acute, recovery, and chronic functions are distributed across regional facilities. Enhanced coordination across these bed functions ensures patients can move smoothly from acute to recovery and chronic care, improving outcomes and reducing staff workload.
The impact on healthcare services
Hospital bed differentiation has several implications for the delivery of healthcare services:
- Greater efficiency
- Improved quality of care
1. Greater efficiency in medical services
The first expected benefit is improved medical service efficiency. Under the current Japanese system, general hospital beds serve different functions depending on the hospital, leading to an unbalanced distribution of medical resources, such as a concentration in acute care. By clearly defining each hospital’s role within the Japanese hospital system, resources can be allocated more efficiently, preventing overconcentration in acute care and ensuring balanced service for patients across all care levels.
2. Improved quality of medical services
With clearer role allocation, hospitals can focus on their designated patient groups. This functional specialization enhances treatment quality, increases capacity for recovery and chronic care, and helps address workforce shortages in Japan.
The impact on pharmaceutical companies
For the pharmaceutical industry, the shift toward differentiated hospital functions directly affects demand for medicines. Each hospital type manages patients with distinct conditions, which alters prescribing patterns and product needs.
As a result, pharmaceutical companies must adapt their strategies, tailoring medical information and product positioning to the specific role of each institution. Beyond medical representatives (MRs), the expertise of Medical Science Liaisons (MSLs) is becoming increasingly valuable.
Another development is the rise of Regional Medical Cooperation Promotion Corporations, authorized entities that coordinate hospitals within a region. These corporations, which are unique to Japan’s healthcare system, can jointly procure pharmaceuticals, making them key customers for international and domestic pharma companies alike.
References:
Ministry of Health, Labour and Welfare, “On the Regional Healthcare Coordination Promotion Corporation System.”
https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177753.html (accessed November 14th, 2023)Ministry of Health, Labour and Welfare, “Overview of the Regional Healthcare Coordination Promotion Corporation System.”
https://www.mhlw.go.jp/file/06-Seisakujouhou-10800000-Iseikyoku/0000205204.pdf (accessed November 14th, 2023)
Impact on patients
One of the defining characteristics of Japan’s acute care hospitals is the “7:1” nursing system, which mandates one nurse for every seven patients in general wards. Hospitals operating under this system must comply with strict rules: maintaining an average length of stay of 18 days or less, ensuring a minimum proportion of high-severity patients, and achieving a home discharge rate of at least 80%.
While these regulations are designed to maintain efficiency and focus resources on the most urgent cases, they also restrict flexibility. For example, cancer patients who could benefit from a longer hospital recovery period are often discharged earlier than they might be in other countries. The requirement to prioritize home discharges over transfers to recovery facilities has also limited options for patients needing intermediate care.
With the advancement of hospital bed functional differentiation, however, patients are beginning to see more treatment pathways. After completing acute care, they now have greater access to recovery and chronic care facilities, as well as outpatient treatment at nearby clinics. These expanded options make it easier for patients and their families—whether through hospital referrals or independent research—to choose care that matches their medical condition and recovery stage.
Ultimately, when patients can continue to receive appropriate medical care beyond acute treatment, the burden on both patients and families is reduced, and the likelihood of smoother recovery outcomes increases.
[Conclusion]
Hospital Bed Reform and Future Outlook
Hospital bed functional differentiation is a healthcare initiative aimed at reorganizing hospital beds into four functional categories: advanced acute care, acute care, recovery care and chronic care. This reform represents a major modernization of the Japanese hospital system. The goal is to improve the efficiency of medical services and enable patients to choose medical care that better suits their individual needs. The government plans to complete this reorganization by 2025 to address key healthcare challenges.
The differentiation of hospital bed functions is expected to lead to an increase in specialized beds for recovery and long-term care, areas where demand is anticipated to grow. It will also allow more efficient allocation of resources aligned with patient needs, while giving patients the option to stay closer to home during treatment. This reform is anticipated to significantly impact healthcare economics, making it essential to monitor these trends closely.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





