The Future of the Health Insurance Claims Database
The healthcare industry is rapidly evolving, with technological advancements driving improvements in efficiency, patient care, and data management. At the core of this evolution is the health insurance claims database, a critical tool used by hospitals, insurance companies, and healthcare providers to manage claims, improve treatment outcomes, and streamline operational processes. As we look to the future, health insurance claims databases are set to become even more integral to the healthcare system, with innovations such as artificial intelligence (AI), blockchain, and predictive analytics poised to reshape how these databases function.
In this article, we will explore the future of the health insurance claims database in the medical industry, how these systems are expected to evolve, and the key technologies that will influence their development.
Contents
- What Is a Health Insurance Claims Database?
- AI and Machine Learning in Claims Databases
- Blockchain for Enhanced Security and Transparency
- Cloud-Based Solutions for Scalability and Accessibility
- Interoperability and Data Standardization
- The Role of Predictive Analytics in Healthcare
- Future Challenges and Ethical Considerations
- Conclusion
What Is a Health Insurance Claims Database?
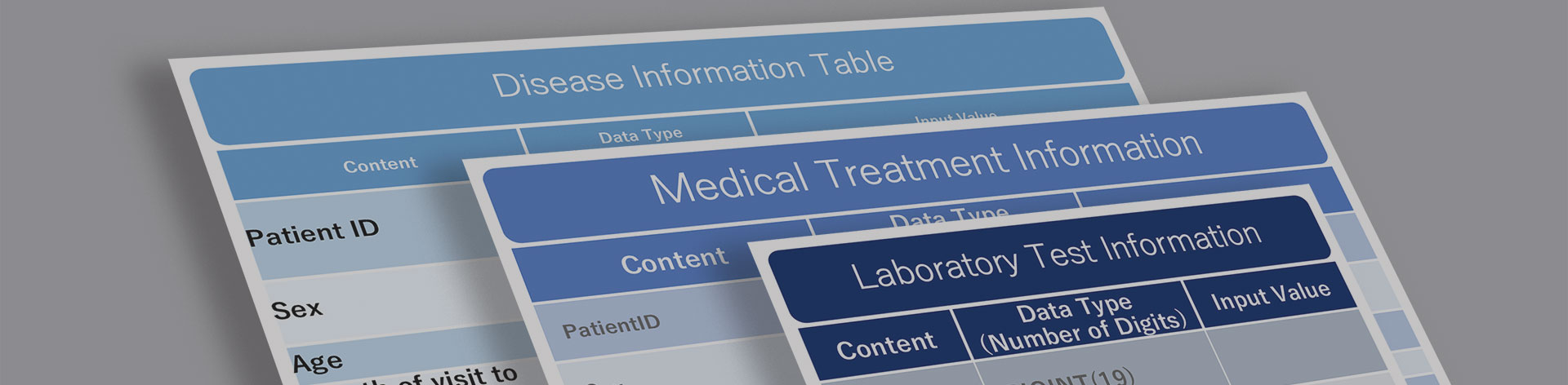
A health insurance claims database is a centralized repository that stores detailed information about patients’ healthcare services, including diagnoses, treatments, medications, and insurance claims. Hospitals and insurance companies use these databases to:
- Process insurance claims: Ensure accurate billing and reimbursement for medical services.
- Track patient care: Document the treatments and procedures provided to patients.
- Analyze healthcare trends: Identify patterns in patient care and insurance claims.
The data stored in these databases is crucial for making informed decisions, optimizing hospital operations, and ensuring that patients receive appropriate care. The future of these databases will be shaped by advances in technology that enhance data accuracy, security, and accessibility.
AI and Machine Learning in Claims Databases
One of the most significant trends shaping the future of health insurance claims databases is the integration of artificial intelligence (AI) and machine learning. These technologies have the potential to revolutionize how claims are processed, how fraud is detected, and how patient care is managed.
Automated Claims Processing
Traditionally, claims processing has been a time-consuming and labor-intensive task. Hospital staff must manually enter data, review claims, and ensure that all necessary information is included. However, with AI-powered systems, much of this work can be automated.
AI can analyze claims data in real-time, flagging errors, inconsistencies, or missing information before a claim is submitted. This reduces the chances of claim denials and speeds up the reimbursement process. AI systems can also learn from past claims data, enabling them to become more accurate over time.
Predictive Analytics and Risk Assessment
In addition to streamlining claims processing, AI and machine learning can be used to predict healthcare trends and assess patient risk. By analyzing historical claims data, these systems can identify patterns that may indicate a patient’s likelihood of developing certain conditions, allowing healthcare providers to intervene earlier and improve patient outcomes.
For example, if a health insurance claims database shows that a patient has a history of diabetes, high blood pressure, and smoking, AI algorithms can assess the patient’s risk of developing heart disease and recommend preventive measures. This proactive approach to healthcare not only improves patient care but also reduces the long-term costs associated with chronic conditions.
Blockchain for Enhanced Security and Transparency
Data security and privacy are major concerns in the healthcare industry, particularly when it comes to handling sensitive patient information stored in health insurance claims databases. As databases continue to grow in size and complexity, the need for robust security measures becomes more important. Blockchain technology offers a promising solution for addressing these challenges.
Decentralized Data Storage
Blockchain is a decentralized technology that allows data to be stored in a distributed ledger, where each record is linked to the one before it, creating a chain of blocks. This ensures that data cannot be altered without leaving a trace, making it nearly impossible for unauthorized parties to tamper with the information.
By implementing blockchain technology, health insurance claims databases can ensure that patient records and claims data are secure, transparent, and easily accessible by authorized parties. This is particularly important in an era where cyberattacks and data breaches are becoming increasingly common. Blockchain can also facilitate real-time data sharing between hospitals, insurers, and other healthcare providers, improving coordination and reducing administrative delays.
Smart Contracts for Automated Payments
Another application of blockchain in health insurance claims databases is the use of smart contracts. These are self-executing contracts that automatically process payments when certain conditions are met. For example, once a claim is approved by the insurance company, the smart contract can trigger an automatic payment to the healthcare provider.
This technology not only speeds up the claims process but also ensures that payments are made accurately and on time. Moreover, smart contracts can help reduce disputes between insurers and healthcare providers by providing a transparent record of the terms and conditions of the contract.
Cloud-Based Solutions for Scalability and Accessibility
As the volume of healthcare data continues to grow, hospitals and insurance companies are increasingly turning to cloud-based solutions to manage their health insurance claims databases. Cloud technology offers several advantages, including scalability, cost-effectiveness, and enhanced accessibility.
Scalability
One of the biggest challenges faced by traditional claims databases is their limited storage capacity. As more patients receive care and file claims, the amount of data that needs to be stored and processed increases. Cloud-based solutions provide virtually unlimited storage, allowing healthcare organizations to scale their databases as needed without investing in expensive on-premise infrastructure.
This is particularly important for large hospital systems that handle thousands of claims each day. By storing their data in the cloud, these organizations can ensure that their databases remain efficient and responsive, even as the volume of claims grows.
Accessibility
Another advantage of cloud-based databases is that they can be accessed from anywhere, at any time. This is particularly beneficial for healthcare providers who need to collaborate with other organizations or access patient records while working remotely. Cloud-based systems also facilitate real-time data sharing, allowing insurers and healthcare providers to quickly access and update claims information, improving efficiency and reducing delays in the claims process.
Interoperability and Data Standardization
One of the ongoing challenges in the healthcare industry is the lack of interoperability between different systems. Hospitals, clinics, insurers, and other healthcare providers often use different software systems to manage patient records and process claims. This lack of standardization can lead to data silos, making it difficult to share information between organizations and slowing down the claims process.
FHIR and HL7 Standards
To address this issue, the healthcare industry is moving toward the adoption of data interoperability standards such as FHIR (Fast Healthcare Interoperability Resources) and HL7 (Health Level Seven). These standards provide a framework for ensuring that different systems can communicate with each other, enabling the seamless exchange of data between health insurance claims databases and other healthcare systems.
By adopting these standards, hospitals and insurers can ensure that patient records and claims data are easily accessible and can be shared between different systems without the need for manual data entry or reconciliation. This not only improves efficiency but also reduces the risk of errors and ensures that patients receive the care they need, regardless of where they seek treatment.
The Role of Predictive Analytics in Healthcare
Predictive analytics has already begun to make a significant impact in the medical field, and its role is expected to expand as health insurance claims databases become more advanced. By analyzing vast amounts of historical data, predictive analytics can identify trends and potential risks, enabling healthcare providers to take a proactive approach to patient care.
Risk Management
For example, hospitals can use predictive analytics to identify patients who are at high risk of readmission after discharge. By intervening early and providing targeted care, healthcare providers can reduce readmission rates and improve patient outcomes. Insurance companies can also use predictive analytics to assess the likelihood of future claims, allowing them to adjust premiums and reduce their financial exposure.
Future Challenges and Ethical Considerations
While the future of the health insurance claims database looks promising, there are several challenges that healthcare organizations will need to address. One of the most significant is the issue of data privacy. As more patient data is collected, stored, and analyzed, ensuring that this information is kept secure and confidential will be critical.
Additionally, the use of AI and predictive analytics raises ethical questions about how this technology should be used. For example, should insurance companies be allowed to adjust premiums based on predictive models that assess a patient’s likelihood of developing a chronic condition? How can healthcare providers ensure that these technologies are used in a way that benefits patients without compromising their privacy or autonomy?
Conclusion
The future of the health insurance claims database in the medical industry is bright, with advancements in AI, blockchain, cloud computing, and interoperability set to transform the way healthcare providers and insurers manage patient data and process claims. As these technologies continue to evolve, health insurance claims databases will become even more essential for improving efficiency, enhancing patient care, and reducing healthcare costs.
However, with these advancements come new challenges, particularly around data privacy and ethics. Healthcare organizations will need to navigate these issues carefully to ensure that the benefits of these technologies are realized while protecting patient rights and maintaining trust in the healthcare system.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





