The Role of Insurance Claims Databases in Enhancing Hospital Operations and Patient Care
In the medical industry, an insurance claims database is more than just a repository for billing data. It plays a critical role in ensuring smooth operations within healthcare organizations, improving patient care, reducing fraud, and optimizing financial and resource management. A comprehensive claims database provides healthcare providers, insurers, and policyholders with a centralized system for managing patient records, tracking medical treatments, and efficiently processing insurance claims. In this article, we will explore the various ways in which an insurance claims database impacts the medical industry, particularly in hospitals, and why it is indispensable for both healthcare and insurance sectors.
Contents
- Efficient Claims Processing and Payment Management
- Enhanced Patient Care and Medical Record Accuracy
- Fraud Detection and Prevention
- Compliance with Regulatory Requirements
- Data-Driven Decision Making and Predictive Analytics
- Cost Reduction and Resource Optimization
- Support for Evidence-Based Medicine (EBM)
- Improved Collaboration between Insurers and Hospitals
- Scalability and Future Growth
- Conclusion
Efficient Claims Processing and Payment Management
At the heart of every hospital’s financial operations is the efficient processing of insurance claims. Hospitals submit claims to insurers for services rendered to patients, and an insurance claims database helps streamline this process by automating data entry, tracking claims status, and managing payment schedules.
When hospitals store patient records and claim information in a unified database, it minimizes the chances of errors and delays. Moreover, integrating such databases with automated billing systems ensures that hospitals can quickly submit claims, track outstanding payments, and reconcile discrepancies with insurers. This also prevents overbilling, underbilling, or claim denials, which can be costly and time-consuming for hospitals to resolve.
For instance, companies like Medical Data Vision (MDV) specialize in providing comprehensive medical claims databases, which are used by over 480 hospitals in Japan to streamline insurance claims processing. MDV’s database integrates patient records and claims data, allowing healthcare professionals to efficiently manage claims while ensuring that patient care is not compromised.
Enhanced Patient Care and Medical Record Accuracy
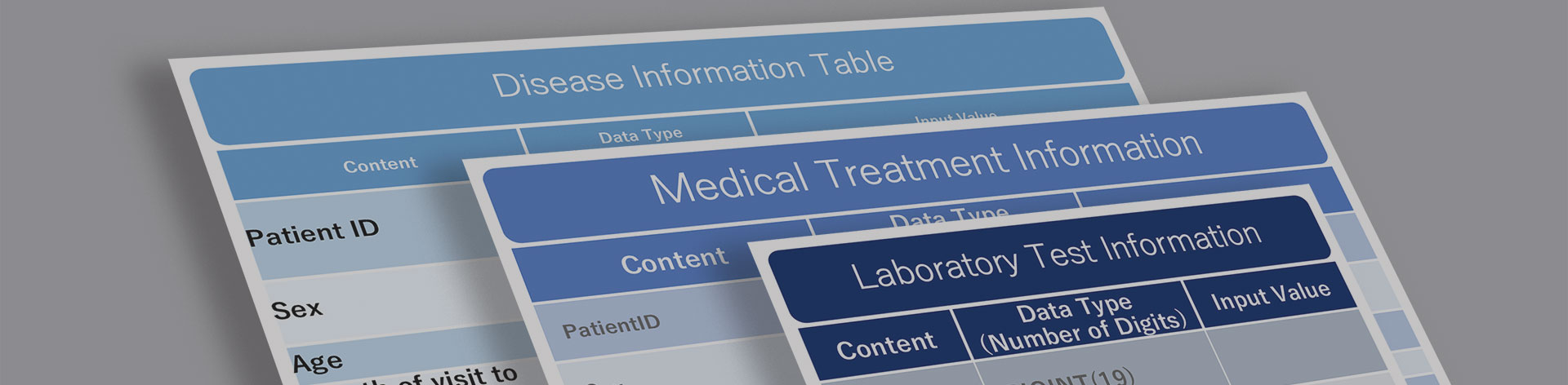
An insurance claims database does more than manage financial transactions; it also plays a key role in improving patient care by integrating patient medical records with insurance data. These databases allow hospitals to store vast amounts of patient information, from personal identification to treatment history, diagnoses, medications, and outcomes. This holistic approach ensures that healthcare providers have access to up-to-date patient records when making treatment decisions.
For example, doctors can easily access past treatments, medical procedures, or test results through the insurance claims database, helping them tailor treatment plans to the patient’s unique medical history. Additionally, insurance data can reveal trends in patient outcomes, such as how patients with similar conditions have responded to different treatment plans, which can further guide healthcare providers in making evidence-based decisions.
By ensuring that patient records are meticulously maintained, insurance claims databases contribute to more personalized care and reduce the likelihood of medical errors, which can arise from incomplete or incorrect data.
Fraud Detection and Prevention
Insurance fraud is a pervasive issue that affects both insurers and healthcare providers. An insurance claims database provides a robust solution for detecting and preventing fraudulent activities by storing and analyzing vast amounts of claims data. When hospitals and insurers collaborate using a shared database, they can identify patterns of suspicious claims that may indicate fraudulent behavior.
Fraud detection mechanisms in these databases often rely on data analytics and machine learning algorithms to flag anomalies. For example, the system can detect when multiple claims are submitted for the same service, or if there is a sudden increase in claims from a particular provider or for specific services. This enables insurers and hospitals to act quickly and investigate potential fraud, saving millions of dollars annually.
The National Healthcare Anti-Fraud Association (NHCAA) highlights that data analytics tools, combined with a well-organized claims database, play a critical role in identifying fraudulent claims and reducing healthcare costs. Hospitals that use such systems can also prevent internal fraud by ensuring that all claims are documented accurately and that there is a proper audit trail for every transaction.
Compliance with Regulatory Requirements
The healthcare industry is heavily regulated, with strict guidelines for patient privacy, data security, and financial transparency. An insurance claims database is essential for hospitals to comply with these regulations, as it provides a central repository for maintaining patient records, billing information, and claims data in a way that meets regulatory standards.
For example, in the United States, the Health Insurance Portability and Accountability Act (HIPAA) mandates strict privacy and security regulations to protect patient data. A well-structured claims database ensures that hospitals can securely store and manage patient information, reducing the risk of data breaches and ensuring compliance with HIPAA regulations.
Moreover, hospitals must regularly submit financial reports and claims data to regulatory authorities. An insurance claims database simplifies this process by providing detailed and accurate records that can be easily retrieved for reporting purposes. This level of transparency is essential for maintaining trust with regulators, insurers, and patients.
Data-Driven Decision Making and Predictive Analytics
A comprehensive insurance claims database allows hospitals and healthcare providers to leverage data-driven insights to improve operational efficiency and patient outcomes. By analyzing claims data, hospitals can identify trends, monitor the effectiveness of treatments, and make more informed decisions regarding resource allocation and staffing.
In addition to supporting operational decisions, these databases can be used for predictive analytics. By analyzing historical claims data, hospitals can predict future trends in healthcare demand, such as seasonal spikes in hospital admissions or the likelihood of certain medical conditions becoming prevalent. This helps hospitals prepare for future healthcare challenges, ensuring that they have the resources, staff, and infrastructure in place to meet patient needs.
Insurance claims databases also help healthcare providers identify areas where they can improve the quality of care. For example, if claims data reveals a high number of readmissions for certain conditions, hospitals can investigate the reasons behind these readmissions and develop strategies to reduce them.
Cost Reduction and Resource Optimization
Managing a hospital’s financial health is a complex task, and an insurance claims database can play a crucial role in reducing operational costs. By automating the claims submission and payment process, hospitals can reduce the administrative burden on staff, allowing them to focus on more critical tasks such as patient care.
Moreover, hospitals can use the insights gained from claims data to identify cost-saving opportunities. For instance, hospitals can analyze data to determine the cost-effectiveness of certain treatments or identify areas where they are spending too much on unnecessary procedures or medications.
Additionally, hospitals can negotiate better reimbursement rates with insurers by presenting data that demonstrates the effectiveness of their treatments and the quality of care provided to patients. This can result in higher reimbursement rates and better financial outcomes for the hospital.
Support for Evidence-Based Medicine (EBM)
Evidence-Based Medicine (EBM) is a medical approach that emphasizes the use of clinical data and research evidence to guide treatment decisions. Insurance claims databases play a vital role in supporting EBM by providing healthcare providers with access to real-world data on patient outcomes and treatment efficacy.
By analyzing claims data, hospitals can identify which treatments are most effective for certain conditions and which procedures result in the best patient outcomes. This information can be used to develop treatment guidelines, improve patient care, and ensure that medical decisions are based on the best available evidence.
For instance, MDV’s claims database allows healthcare professionals to access real-time data on patient outcomes, helping them make informed decisions based on evidence from actual patient cases. This integration of data supports the broader goals of precision medicine, which aims to provide personalized treatment plans that are tailored to the specific needs of individual patients.
Improved Collaboration between Insurers and Hospitals
The relationship between hospitals and insurers is often complex, with both parties needing to collaborate closely to ensure that patients receive the care they need while keeping costs manageable. An insurance claims database facilitates better communication and collaboration between hospitals and insurers by providing a shared platform for managing claims, tracking payments, and resolving disputes.
This centralized approach reduces the likelihood of misunderstandings or miscommunication, as both parties have access to the same data and can work together to resolve issues. In addition, the transparency provided by a claims database ensures that both hospitals and insurers can track the status of claims and payments in real-time, reducing delays and improving efficiency.
Scalability and Future Growth
As the healthcare industry continues to grow and evolve, hospitals need systems that can scale with their operations. An insurance claims database provides the scalability needed to manage increasing volumes of patient data and insurance claims.
With the rise of cloud-based solutions, hospitals can now store and manage vast amounts of data without the need for expensive on-site infrastructure. This scalability allows hospitals to expand their operations and accommodate new patients without worrying about data storage limitations.
Moreover, as hospitals adopt new technologies such as artificial intelligence (AI) and machine learning, an insurance claims database provides the foundation for integrating these technologies into their operations. AI and machine learning can be used to analyze claims data, predict future trends, and improve the accuracy of diagnoses and treatment plans.
Conclusion
In conclusion, an insurance claims database is an invaluable asset for hospitals and healthcare providers. From streamlining claims processing and improving patient care to detecting fraud and ensuring regulatory compliance, these databases play a crucial role in the efficient functioning of the healthcare industry.
By leveraging the power of data, hospitals can make informed decisions, improve patient outcomes, and ensure that they are delivering high-quality care at a reasonable cost. As the healthcare industry continues to evolve, insurance claims databases will become even more critical in supporting the growth and success of hospitals around the world.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





