Note: The opinion of the author expressed in the article does not represent any official opinion or position of Medical Data Vision regarding the 2022 Reform of the Medical Fees. The series of article is designed to provide insight and matter to discuss the healthcare environment among various stakeholders. Thanks for your understanding.
2006 is the year marking the pivotal change introducing the “Comprehensive Community Care System” as the central part of the 5th Revision of the Medical Care Act promulgated in June 2006 and enforced from April 2007. The Government set a clear objective by 2025 to create a system that would comprehend housing, medical care, long-term care, prevention, and life support in an integrated manner that laid the foundation of the current medical flow. The key concern was to prepare the country’s infrastructures to cope with the baby-boomers’ generation reaching 75 years old by 2025. 16 years have passed since then and we can measure in our daily life that community medicine has become a reality with new concepts such as “family doctors” or “assigned pharmacies”. As the target date approaches, it is time to measure the progress and the gap and reflect on the incoming changes to expect.
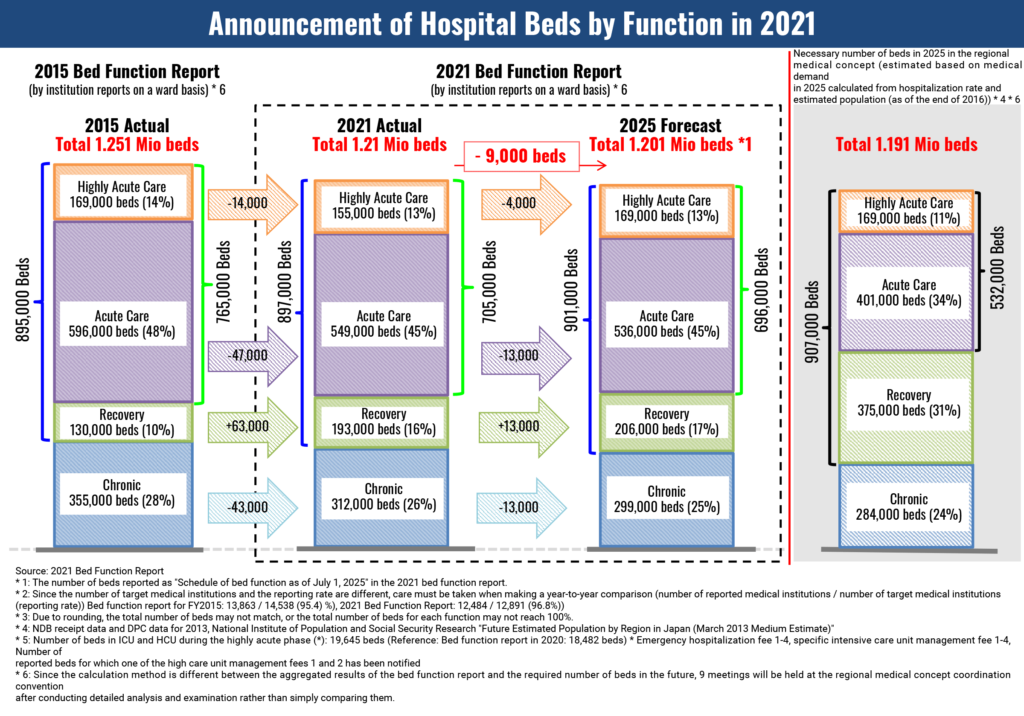
The Government made the transition very clear in the report of the National Conference on Social Security System Reform in August 2013. The goal is to move from “Hospital-driven medical care focusing on life-saving or life prolongation, healing and rehabilitation” to a new medical care concept centered upon “the area, the home where citizens are accustomed to live”. The Ministry of Health, Labor and Welfare’s (MHLW) intention to shift to “community-based” medical care is progressively making roots but it is hard to evaluate how robust the implementation is going. Some recent publications about the changes in the number of hospital beds and the resource allocation between each medical function at the hospital are very valuable hints at the way MHLW is thinking about the future.
Working Group on the 5th Community Healthcare Initiative and Doctor Recruitment Plan “Regarding the implementation of the bed function report in 2022”
The Government has set the upper limit for overtime work as part of its “Working Style Reform” and the resolution is to expand the rules to medical doctors from April 1, 2024. Each medical institutions are likely to be monitored for taking serious measures of enforcement at this occasion. It is commonly referred to as the “2024 Problem” and ranks on top of hospital management priorities right now. This mechanism to limit the working hours of doctors within this Labor Law Reform has been fully embedded into the 5th Revision of the Medical Care Act of 2006. Back then, experts referred to “not too distant future” but it is now around the corner.
It may not seem obvious but in our understanding, the reorganization of hospital beds and the “reform of doctors’ working styles” are what exactly represents the “comprehensive community care system” and justify its implementation.
Among the acute care hospitals, doctors in all hospitals continue to treat day and night critically ill patients and are returning patients to their homes while being forced to meet the requirements for shorter length of stay. On the other hand, convalescent hospitals spend a lot of time caring for patients, up to when doctors and patients are well prepared to return home. If longer-term treatment is required, it is ideal that nurses and specialized staff stand at the receiving end more than doctors in the medical ward, to help patients get back their independence to be sent home. This reallocation of resources and expertise while realigning the goals and purpose of treatment already formed the core of the 2014 Medical Fees Reform.
However, the so-called “community comprehensive care ward” often settled in acute care hospitals, diverting the original sense that “community comprehensive care ward” could provide homecare and standard medical care differently. The 2022 Medical Fees Reform intended to address this deviation from the initial purpose set forth in 2014, by seriously tightening the requirements for each medical institution. Such fluctuations in the implementation and running of a new healthcare structure show how much MHLW is willing the reaffirm the direction of the regional medical care reform. We surely witness a shift from “hospital-driven” to “community-driven” healthcare.
Put into such a perspective, it appears that the “comprehensive community care system” attempts to move patients according to the treatment phase. This is probably the biggest “task share” challenge faced by medical institutions for the time being.




