Note: The opinion of the author expressed in the article does not represent any official opinion or position of Medical Data Vision regarding the 2022 Reform of the Medical Fees. The series of article is designed to provide insight and matter to discuss the healthcare environment among various stakeholders. Thanks for your understanding.
“Concept of Medical Community” and “outpatient function reporting system”
In May 2021, when the number of newly infected people with the new coronavirus reached its fourth peak, the Japanese Government undertook to reform the Medical Care Act with new legislation, officially “a system to efficiently provide high-quality and appropriate medical care” and “to promote the securing of medical care”. The new Law was passed and issued on May 28 with the goal to strengthen support for the working styles of doctors and the realization of regional plans for medical care.
Originally, the 6th Medical Plan (Notice of the Director of Medical Affairs Bureau, Ministry of Health, Labor and Welfare on March 30, 2012) talked about measures to promote the differentiation and cooperation of medical institutions, and the 7th Medical Plan (March 31, 2017 – Notice of Director of Medical Affairs Bureau, Ministry of Health, Labor and Welfare) included remarks on efforts to achieve the “medical community concept” formulated by each prefecture at the end of 2016.
At first glance, this law, which indicates that necessary amendments will be made to carry out this “medical community concept”, included measures for reforming the working styles of doctors and a review of the work description for medical staff. The first impression was that the legislation was highly guided by human resource considerations, but in reality, it proved far more complex, challenging the initiative to reform the hospital bed reorganization by function in 2020 as well. The 2020 Reform on Medical Fees and tax treatment for medical institutions went into the very same direction indeed.
It made necessary the definition of a framework to provide preferential treatment and to strengthen the cooperation between medical functions for outpatient, the establishment of a policy that requires reporting on outpatients that preferentially utilize medical resources.
Through this process, the outpatient function reporting system was finally put into effect in April this year.
In fact, this outpatient function reporting system is simply called “reporting system”, but unlike the former “bed function reporting system”, medical institutions do not collect medical data by themselves to report the statistics. “Based on the items that can be grasped in the general information database (also known as National Database or “ NDB ”) such as receipt information and specific medical examinations, the medical institution side responds to the survey by the medical institution’s” outpatient department that manages the medical resources. The motivation to respond to the Prefectural governor is in proportion with the intention of “gaining the status of a medical institution that plays a key role in the region.”
In addition, the medical institutions subject to reporting obligations are not limited to hospitals, but also clinics that intensively carry out examinations using expensive medical equipment for example, so the attitude toward this system and the Ministry of Health, Labor and Welfare is both a matter of motivation and commitment to the medical regional concept.
On the other hand, we should note that the use of public data such as NDB for the aggregated results may look like a great story of workload reduction for hospital administration, but it also obliterates any consideration for patients and the doctors who do not appear in the data, so it is fair to assume that the initial ideal of humanistic medicine is not entirely reflected.
“Family doctor” / “Priority doctor for referral consultation”
Each medical institution will be screened based on data to a certain extent within the outpatient function reporting system, but the final decision is left to the medical institution.
By raising the hand to become a “priority medical institution for referral consultation”, that will somewhat form a “tag” as “community medical support hospital” to make it a medical institution that “focuses on utilizing medical resources” in the region, and it will be a facility that provides advanced medical care.
It is necessary to make a choice as to whether to position the facility as a “family doctor” and provide medical care in a form closely related to the community, and to create a relationship where the faces of patients and medical personnel who are closely related to the community can be seen. There is a fair balance between proximity to patients and providing sophisticated medical care. Now that not only medical staff but also those who receive medical care are required to get rid of the heavy equipment hospital consultation, “family doctors” will play a central role in promoting awareness change and shortening the distance with citizens. I think that is the first step in building a comprehensive community care system.
By the way, in the working style reform for doctors, various measures have been greatly highlighted, such as introducing refill prescriptions for doctors in clinics and entrusting medication guidance and residual drug management to pharmacists. However, we should keep in mind that the system for reducing the work of doctors has been expanded.
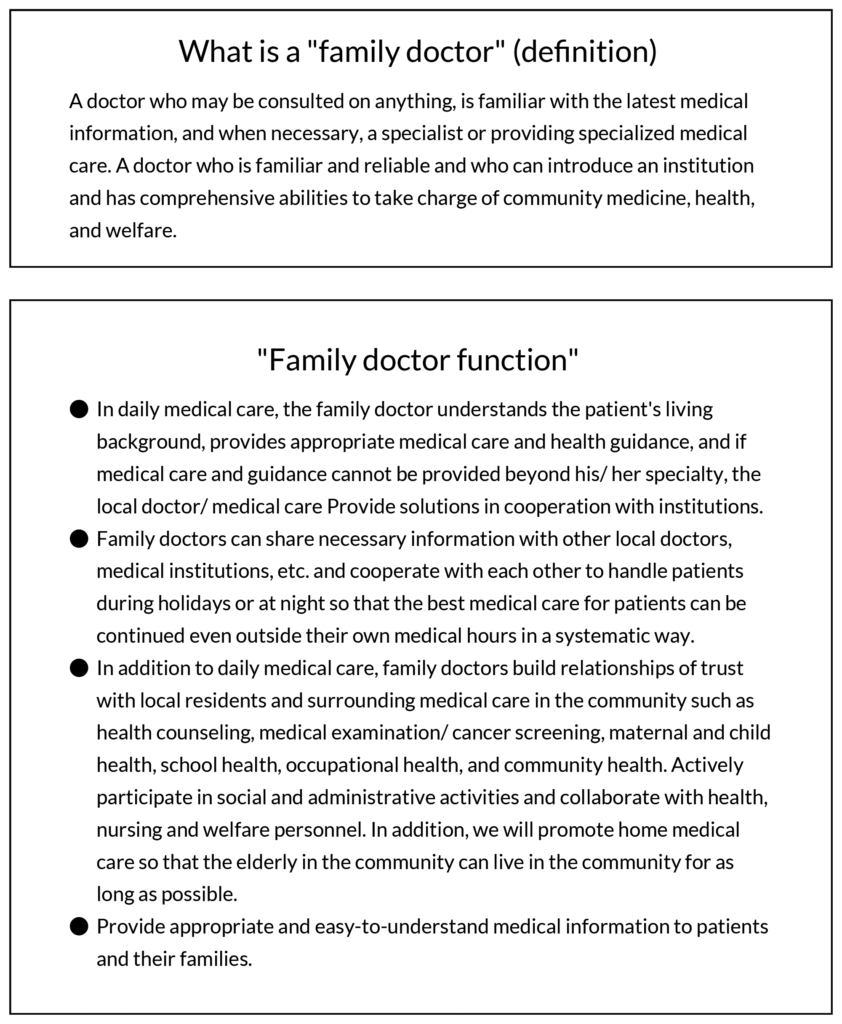
Source: “The ideal medical care delivery system” Joint proposal by the Japan Medical Association and the Four Hospital Group Council (August 8, 2013)
10th Meeting of the Study group on the 8th Medical Plan related to family doctor function