How Does a Medical Claims Database Work in Healthcare?
Medical claims databases are at the heart of today’s healthcare system. Hospitals, insurers, and healthcare providers rely on these systems to store, manage, and process claims, while ensuring that patient care remains at the forefront. A medical claims database stores comprehensive information, including patient records, billing data, and claims information, facilitating the smooth operation of healthcare and insurance systems.
This article explains in detail how a medical claims database works, focusing on the medical industry, especially hospitals that use it for patient care and insurance claims processing. The database allows healthcare professionals to improve efficiency, reduce administrative costs, and enhance patient care by leveraging accurate and comprehensive data.
Overview: What Is a Medical Claims Database?
A medical claims database is a digital repository that stores detailed information about patients’ medical treatments, diagnoses, and procedures, as well as the insurance claims associated with these services. This data is typically used by hospitals, clinics, insurers, and regulatory bodies to:
- Track patient care: Document the treatment provided, diagnoses made, and medications administered.
- Manage claims: Streamline the insurance claims process and reduce administrative overhead.
- Analyze healthcare trends: Provide insights into healthcare patterns and assist in policy development.
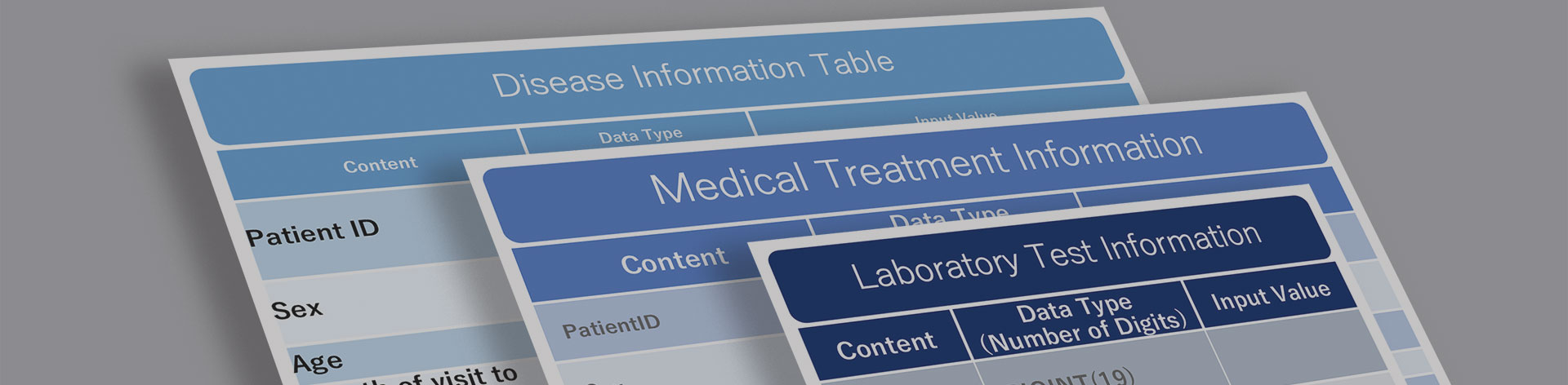
The structure of a medical claims database usually includes several key data points:
- Patient Demographics: Name, age, gender, and contact details.
- Medical History: Diagnoses, lab results, prescriptions, and treatments.
- Insurance Claims Data: Dates of service, provider details, service costs, and claims status.
These databases are critical for managing healthcare operations and ensuring smooth communication between hospitals and insurance companies.
How Medical Claims Database Systems Work
At its core, the medical claims database functions as an integrated system that brings together patient records and insurance data. The system is designed to ensure that healthcare providers can document the services they provide, while insurance companies can quickly and efficiently process the claims associated with these services. Here’s a breakdown of how these systems work:
Data Collection
When a patient visits a hospital, the medical claims database begins by collecting a wealth of information about their condition, treatment, and any subsequent actions. This includes:
- Diagnoses made by healthcare professionals.
- Tests conducted, such as X-rays or bloodwork.
- Treatments prescribed, such as medications or surgeries.
- Details of follow-up care, if any.
Simultaneously, the system records data related to insurance claims:
- The type of insurance coverage the patient has.
- The cost of the treatments provided.
- The claims filed with the insurance company.
All of this data is entered into the system and stored securely, allowing both healthcare providers and insurers to access it as needed.
Claims Submission
Once the necessary information is collected, the hospital submits a claim to the patient’s insurance company. This is often done electronically, with the medical claims database automatically generating the claim based on the information that was entered at the time of the patient’s visit. The system ensures that all necessary information is included, such as procedure codes (ICD, CPT) and cost breakdowns, making the process faster and reducing the chance of errors.
The claim is then sent to the insurer for processing. Insurance companies use the information stored in the medical claims database to verify the details of the claim and determine how much of the cost will be covered under the patient’s insurance policy. This process is known as claims adjudication.
Claims Adjudication
After receiving the claim, the insurance company uses algorithms and automated systems to verify the accuracy of the information provided. The medical claims database plays a critical role here, as it allows the insurer to cross-reference the claim with previous claims data, as well as the patient’s policy details. This helps determine:
- Whether the treatments provided are covered under the patient’s insurance plan.
- How much of the cost will be paid by the insurance company.
- Whether there are any outstanding issues or discrepancies that need to be resolved before payment can be made.
At this stage, the insurer may request additional information from the hospital, such as documentation of the treatment provided, or details about why a particular procedure was performed.
Payment Processing
Once the claim has been adjudicated, the insurer sends a payment to the hospital, covering the agreed-upon portion of the cost. The medical claims database tracks this payment, ensuring that the hospital is compensated for the services provided. It also generates records of the transaction, which are stored for future reference and reporting.
In cases where the insurance company denies a claim, the system provides information on the reasons for the denial, allowing hospitals to address the issue and resubmit the claim if necessary.
The Importance of Medical Claims Databases for Hospitals
Hospitals benefit significantly from using a medical claims database. These systems streamline administrative processes, reduce the likelihood of errors, and free up healthcare professionals to focus on providing high-quality patient care. Here are some of the key advantages:
1.Improved Efficiency
A medical claims database reduces the amount of manual work required to process insurance claims, which speeds up the overall process. This is particularly important for large hospitals that handle thousands of claims each month. By automating many of the steps involved, these databases help healthcare providers submit claims more quickly, reducing the time it takes to receive payment from insurers.
In addition, a well-organized database makes it easier for hospital staff to track the status of claims, ensuring that no payments are missed and that outstanding issues are resolved promptly.
2.Cost Reduction
By improving the efficiency of the claims process, a medical claims database can significantly reduce administrative costs. Hospitals spend less time on paperwork, allowing them to allocate more resources to patient care. Furthermore, the system helps prevent errors, which can be costly to correct and may lead to delays in payment.
3.Regulatory Compliance
Healthcare is a heavily regulated industry, and hospitals must comply with a wide range of laws and guidelines when it comes to managing patient data and processing insurance claims. A medical claims database helps ensure compliance by keeping detailed records of all claims and payments, as well as the treatments and procedures that were provided to patients.
Many databases also include audit trails, which document who accessed the system and what changes were made. This makes it easier for hospitals to demonstrate compliance during audits and avoid penalties.
4. Fraud Detection and Prevention
One of the most important uses of a medical claims database is in the detection and prevention of fraud. Healthcare fraud is a significant issue in the medical industry, and it can cost hospitals and insurers millions of dollars each year. A medical claims database helps reduce fraud by providing detailed records of every claim that is submitted, making it easier to identify suspicious patterns and anomalies.
Pattern Recognition
By analyzing the data stored in a medical claims database, hospitals and insurers can identify patterns that may indicate fraudulent activity. For example, if a provider consistently submits claims for high-cost procedures that are not medically necessary, this could be a red flag. Similarly, if a patient submits multiple claims for the same treatment within a short period, this may warrant further investigation.
Collaboration with Insurers
The medical claims database also allows hospitals to collaborate more effectively with insurers to detect and prevent fraud. By sharing data in real-time, both parties can quickly identify and address potential issues before they escalate. This helps protect the integrity of the healthcare system and ensures that resources are used appropriately.
5. Predictive Analytics and Data-Driven Decision Making
One of the most exciting developments in healthcare is the use of predictive analytics to improve patient outcomes and reduce costs. A medical claims database provides the foundation for these efforts by supplying the data needed to identify trends and make informed decisions.
Predictive Models
Using the data stored in a medical claims database, hospitals can develop predictive models that help forecast future healthcare needs. For example, by analyzing historical claims data, hospitals can predict when certain types of illnesses are likely to occur, allowing them to allocate resources more effectively.
These models can also be used to identify high-risk patients and intervene early to prevent complications, improving patient outcomes and reducing costs.
Data-Driven Decision Making
By providing access to a wealth of data, medical claims databases empower hospitals to make data-driven decisions. For example, hospitals can use claims data to analyze the effectiveness of different treatments, identify areas where costs can be reduced, and improve overall patient care.
Conclusion
A medical claims database is a critical tool in the healthcare industry, offering numerous benefits to hospitals, insurers, and patients alike. By streamlining claims processing, reducing administrative costs, preventing fraud, and supporting data-driven decision-making, these systems help ensure that healthcare providers can deliver the best possible care while managing costs effectively.
As healthcare continues to evolve, the importance of medical claims databases will only grow. Hospitals that invest in these systems will be better equipped to handle the challenges of the modern healthcare landscape, improving outcomes for both patients and providers.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





