Advancing Diabetes Care with Insurance Claim Data
Index
Key Takeaway
Insurance claim data has an important role in advancing diabetes care by supporting every stage of patient management, from early diagnosis to personalized treatment and complication prevention. By providing real-world insights into patient health patterns, claims data gives healthcare providers the ability to make more informed decisions that enhance care quality and outcomes. This data helps tailor treatment plans, monitor patient progress, and proactively address potential complications.
Diabetes, especially type 2 diabetes, presents a very significant public health challenge in Japan. The country faces a high prevalence of diabetes, largely driven by aging demographics and lifestyle changes. This condition has far-reaching impacts on the Japanese healthcare system, affecting both economic resources and patient quality of life. As diabetes requires ongoing management, its financial burden on healthcare services can be quite substantial, from frequent medical consultations to the high cost of long-term medications.
Insurance claim data is an important resource for understanding the scope and specifics of diabetes care in Japan. By analyzing claims data, healthcare providers, device manufacturers, pharmaceutical companies, and policymakers can gain a clear picture of how diabetes affects various population groups, where treatment adherence might be falling short, and how healthcare services are being used. This information is essential for creating better management strategies and ensuring that resources are directed toward areas of greatest need, ultimately enhancing care and reducing the long-term impact of diabetes on patients and the overall healthcare system as well.
Understanding Insurance Claim Data and Its Value in Diabetes Care
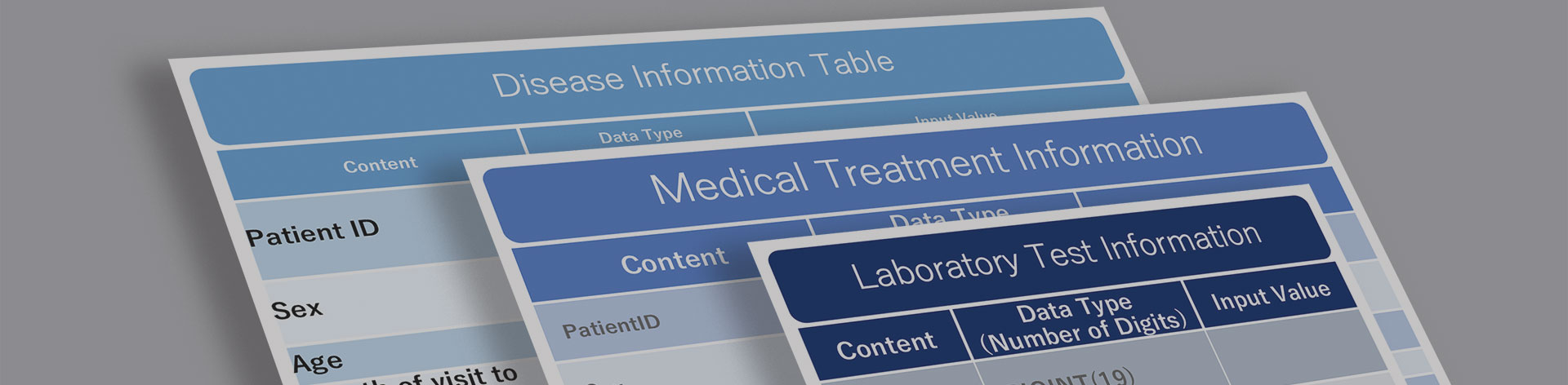
Insurance claim data is made up of records that are submitted by healthcare providers to insurance companies, detailing the treatments, diagnoses, medications, and services used by patients. In chronic diseases like diabetes, claims data provides valuable information on patterns in treatment, medication adherence, and rates of complications. For instance, it allows providers to observe how often patients refill prescriptions, which can indicate adherence to medication regimens. By identifying gaps in medication adherence, healthcare teams can intervene early to support patients and help them better follow their prescribed treatments.
Insurance claim data also offers insights into treatment patterns and the long-term management of diabetes, including trends in hospitalization rates, outpatient visits, and the use of preventive services. These insights are especially beneficial for healthcare providers that want to improve diabetes care. Researchers and policymakers also benefit from access to this data, because it allows them to analyze how effective the current treatment approaches are, and make informed decisions on public health initiatives. For example, policymakers can use claims data to better allocate resources, supporting initiatives that promote lifestyle changes or increase access to early screening programs.
By maximizing insurance claim data, stakeholders can improve outcomes in diabetes care, ensuring that patients receive continuous support that is specifically tailored to their needs. The comprehensive view that claims data provides helps all parties involved make more informed decisions that enhance the quality of care for anyone living with diabetes.
How Insurance Claim Data Supports Early Diagnosis and Monitoring in Diabetes
Insurance claim data plays an important role in the early diagnosis and ongoing monitoring of diabetes. By analyzing patterns in outpatient visits, diagnostic codes, and common risk factors of the disease, healthcare providers can identify people who may be at a higher risk of developing diabetes. This allows for earlier interventions, which can delay or prevent the onset of diabetes. For example, frequent visits for blood sugar tests or weight management consultations may signal a prediabetic condition which could prompt providers to recommend certain lifestyle changes or preventive treatments.
Over time, insurance claim data also helps in tracking the health status of patients as they progress from prediabetes to diabetes. This data allows for continuous monitoring, allowing providers to respond to the ever-changing needs of their patients. Patterns of high blood sugar levels or increased medication use can indicate disease progression, allowing healthcare teams to adjust treatment plans and reduce the likelihood of complications. For instance, if claims data reveals that a patient is consistently using higher doses of diabetes medications, it may suggest that their condition is worsening, prompting more intensive management.
In addition to supporting early detection, insurance claim data is invaluable for establishing preventive measures. By examining how and when complications develop in diabetic patients, providers can introduce targeted interventions in an attempt to reduce the risk. For example, if claims data shows that a particular group of patients frequently experiences kidney issues, providers can recommend regular screenings for kidney function as part of routine diabetes management. These insights from insurance claims help to create more proactive and preventive diabetes care strategies, which ultimately improve long-term health outcomes and reduce the healthcare costs that are associated with advanced diabetes complications.
Personalizing Diabetes Treatment Through Insurance Claim Data
Insurance claim data empowers healthcare providers to develop tailored treatment plans that respond to the specific needs of each individual diabetes patient. By analyzing real-world data, providers can determine which therapies prove most effective across different patient demographics. This gives them the opportunity to adjust treatment approaches based on age, gender, comorbidities, or other factors that may have an influence on treatment outcomes.
One important application of insurance claim data in diabetes care is tracking the efficacy of medication. With diabetes patients often needing long-term insulin or oral medication therapy, monitoring which medication combinations provide the best results is very important. Insurance claims give providers the ability to observe how patients respond to various different treatments over time, identifying those who might benefit from higher or lower dosages. If data shows that patients with similar profiles achieve better blood sugar control with specific medication adjustments, providers can apply these insights to similar cases.
For example, insights from insurance claim data might reveal that certain patient groups achieve more stable glucose levels with a combination of insulin and a particular oral medication. By applying this information, providers can adjust treatment plans to enhance blood sugar control and reduce the risk of complications. Personalized treatment adjustments, guided by claims data, allow for more proactive diabetes management and better patient outcomes.
Leveraging Insurance Claim Data for Better Outcomes in Complications and Long-Term Management
Insurance claim data plays an important role in managing diabetes-related complications, such as neuropathy, retinopathy, and cardiovascular issues. By analyzing claims data, healthcare providers gain a holistic view of a patient’s history, including patterns of recurrent issues, prescription changes, and hospitalization needs. This broad perspective allows providers to anticipate complications before they worsen, making it possible to intervene early.
For instance, if insurance claim data shows a trend of frequent emergency visits because of cardiovascular complications in certain diabetic patients, healthcare teams can incorporate preventive cardiovascular monitoring into their regular diabetes care. This proactive approach helps to reduce hospitalizations and improves the overall quality of life for patients.
Using insurance claim data in this way allows providers to develop strategies that prevent complications from escalating. Long-term management can be refined based on insights from past claims, giving providers the ability to support stable health outcomes and address high-risk factors as they arise. By tracking these data points, healthcare teams can adapt their care plans, ensuring patients with diabetes maintain a better quality of life while minimizing hospitalizations and intensive care requirements.
Insurance Claim Data for Research and Policy Development in Diabetes
Insurance claim data is a very powerful asset in diabetes research, offering large-scale insights into prevalence, treatment patterns, and effectiveness across different populations. Researchers can analyze claims to identify trends in how diabetes affects various demographic groups, track which treatments provide the most favorable outcomes, and evaluate the cost-effectiveness of interventions.
The value of insurance claim data also extends to policymaking, where it helps to inform strategies that enhance the quality and accessibility of diabetes care. Policymakers can use claims data to design initiatives that support early diagnosis, improve treatment accessibility, and encourage preventive care. For example, if data shows low utilization of preventive screenings in certain areas, policies can be developed to promote these screenings and increase awareness.
Plus, insurance claim data helps guide public health programs and resource allocation by highlighting areas of greatest need. Claims data allows for more efficient distribution of resources, addressing specific healthcare needs in diabetes prevention and care. By taking advantage of the available claims data insights, policymakers and healthcare providers can make informed decisions that align with the needs of the diabetic population, ultimately promoting better health outcomes and resource management.
The Future of Diabetes Care Using Insights from Insurance Claim Data
The role of insurance claim data in transforming diabetes care and management is quite profound. By allowing early diagnosis, supporting personalized treatment, and enhancing long-term patient monitoring, claims data is essential for improving healthcare outcomes. In Japan, where comprehensive datasets are available, the impact of claims data on managing chronic diseases like diabetes is especially significant. The Japanese healthcare system, with its structured and thorough data collection practices, provides an invaluable foundation for understanding and addressing the complexities of diabetes care, especially in aging populations.
MDV Database provides extensive data resources that harness the power of insurance claim data to support meaningful advancements in diabetes treatment and research. With its deep commitment to data accuracy and healthcare support, MDV helps healthcare professionals and researchers make informed decisions that enhance patient care and outcomes. For stakeholders interested in improving diabetes care, MDV is a valuable partner, providing the data-driven insights that are needed to make lasting improvements. Contact MDV to learn more about how their data solutions can support your goals in diabetes management.
Frequently Asked Questions
How does data analytics impact insurance claims management?
Data analytics significantly improves insurance claims management by allowing companies to identify patterns and trends in claims, which helps in detecting potential fraud, predicting future claims costs, and optimizing resource allocation. Analytics also reduces operational costs by streamlining claims processing, minimizing errors, and ensuring that claims are handled more efficiently and accurately, ultimately benefiting both insurers and patients.
What is claims data?
Claims data is made up of the records that healthcare providers submit to insurance companies for reimbursement. These records include detailed information about patient diagnoses, treatments, prescribed medications, and healthcare utilization. Claims data offers a comprehensive view of a patient’s healthcare journey, serving as a valuable resource for understanding treatment outcomes, assessing the effectiveness of healthcare services, and supporting data-driven decision-making in healthcare management.
How can insurance companies use claims data?
Insurance companies use claims data to monitor the effectiveness of treatments, assess healthcare service usage, and gather insights that enhance overall healthcare quality. By analyzing claims data, insurers can identify high-risk populations, adjust coverage policies, and develop targeted health programs. This data-driven approach helps insurers improve service quality, reduce costs, and ensure that patients receive appropriate care in a timely manner.
Can insurance companies see your claim history?
Yes, insurance companies can access your claim history. This access allows them to verify previous healthcare services, understand treatment patterns, and assess patient needs for future care. Reviewing claim history also helps insurers manage risk, set premiums, and provide better support by understanding each patient’s specific healthcare background and ongoing requirements.
What are the sources of data in insurance companies’ claims?
The primary sources of data in insurance claims include hospitals, clinics, outpatient centers, and pharmacies. Each source provides important information on patient interactions with healthcare services, including diagnoses, treatments, prescriptions, and healthcare costs. This data allows insurers to gain a complete understanding of patient health and helps them make informed decisions on coverage and care management.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





