News
Analysis of factors influencing length of hospital stay after gastric cancer surgery using medical big data Development of a predictive model with prediction error within 3 days
- December 15, 2025
A research team led by Dr. Tsunehiko Maruyama, Director of the Digestive Disease Center at Mito Saiseikai General Hospital in Mito City, Ibaraki Prefecture, analyzed one of the largest medical databases in Japan owned by Medical Data Vision Co., Ltd. (Chiyoda Ward, Tokyo; President and Chief Executive Officer Hiroyuki Iwasaki, hereafter MDV) using machine learning techniques and developed a model that predicts postoperative length of hospital stay with an error of within three days. The study also found that factors such as whether a hospital is designated as a cancer care center and the size of the hospital are associated with the length of hospital stay for gastric cancer surgery.

Dr. Maruyama
of the research team
The paper reporting this research has been published in Frontiers in Medical Technology.
The original article is available at the following link → https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1732580/full
QR code of
the paper

The MDV medical data analyzed using a machine learning method known as XGBoost included 284,953 cases of gastric cancer recorded over a five year period from August 2017 to July 2022. Of these, 26,299 cases involved patients who underwent surgery. After excluding cases in which patients died within seven days, as well as cases involving patients aged 18 years or younger or 100 years or older, a total of 26,097 cases were included in the analysis. A machine learning model was developed to predict postoperative length of hospital stay based on patient characteristics at the time of admission.
By calculating the relative importance of patient characteristics at admission and identifying factors that influence length of hospital stay, the study succeeded in developing a model that predicts postoperative length of hospital stay with an error of within three days using only patient related factors available at admission. This model may be applied in the future to bed control management.
The factor with the highest relative importance was laparoscopic distal gastrectomy. Among surgical procedures, open total gastrectomy also ranked highly. In addition, institutional factors such as the presence or absence of designation as a cancer care center and hospital size were identified as influential. Patient related factors including activities of daily living score at admission, the scale for assessing independence in daily living among older adults with dementia, and the presence or absence of eating or swallowing dysfunction were also important. Furthermore, comorbidities such as diabetes mellitus, alcoholic hepatitis, post cerebral infarction status, and anxiety disorders were ranked among the top contributing factors.
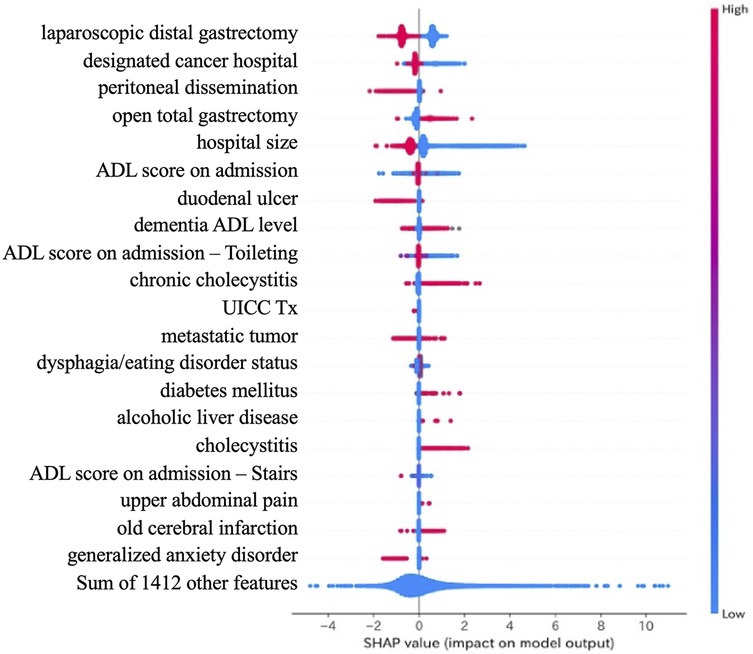
Figure 3. SHAP summary plot for feature interpretability. SHAP (SHapley Additive exPlanations) values visualize the influence of each feature on the model’s output across all patients. Each dot represents an individual patient. Red dots indicate higher feature values, while blue dots indicate lower values. Features are ranked by overall impact. Laparoscopic surgery and large hospital size were associated with shorter length of stay, while open total gastrectomy contributed to prolonged hospitalization.