Transforming HIV Care with Insights from Health Claims Data
Index
Key Takeaway
Health claims data is essential for advancing HIV treatment by allowing for personalized care, improving medication adherence, and enhancing care quality. Using this data responsibly maximizes its potential for improving patient outcomes and strengthening healthcare strategies. This approach ensures that HIV patients receive the most effective, tailored care possible, helping to support their long-term health and well-being.
In healthcare, the use of health claims data is becoming increasingly important for advancing chronic disease management, especially in areas like HIV care and antiviral treatment. This data provides a very detailed view of patient demographics, treatment histories, and healthcare patterns, allowing providers and researchers to make more informed decisions that enhance patient outcomes. By capturing real-world insights, health claims data allows healthcare teams to evaluate treatment efficacy, understand adherence trends, and track patient responses over time. In Japan, where datasets are very comprehensive, health claims data is particularly valuable. Resources like MDV’s extensive database can significantly contribute to HIV research, guiding improvements in patient care and offering critical insights that support effective management and innovation in HIV treatment. This data-driven approach is helping to build more accurate care models and personalized treatment plans, ultimately transforming HIV care for both patients and providers.
Understanding Health Claims Data and Its Value in HIV Care
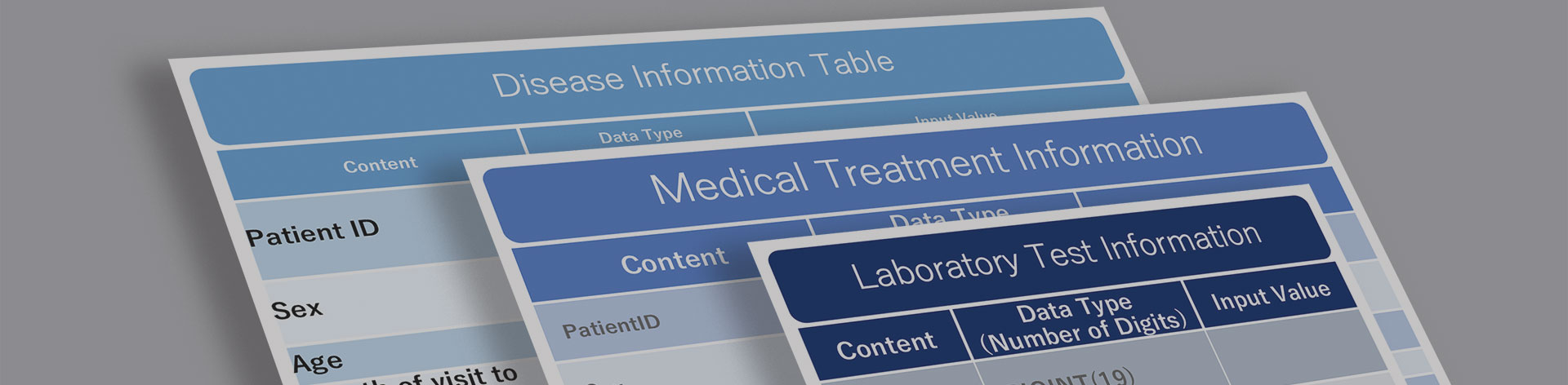
Health claims data is a very comprehensive source of information that records all of the interactions between patients and healthcare providers. This data captures essential details about patient demographics, diagnostic codes, treatments that have been administered, and medication use. For patients with chronic conditions like HIV, health claims data plays an important role in providing a complete picture of their entire healthcare journey. It allows healthcare teams to monitor patient care patterns over a period of time, observe changes in health status, and ensure that treatments align with individual needs.
When it comes to HIV, health claims data can be especially valuable for helping to provide a better understanding of how patients are using antiviral medications. This data reveals adherence patterns, showing whether patients are filling their prescriptions consistently and whether they are properly taking the prescribed dosage. By tracking antiviral use, providers can identify gaps in adherence, which is an essential component in HIV treatment. Consistent medication is critical for suppressing viral loads and preventing resistance. Health claims data also highlights which antiviral treatments show the best outcomes across different patient demographics, helping providers tailor care to enhance its efficacy and reduce any potential side effects.
Plus, health claims data offers healthcare providers, researchers, and policymakers unique insights that support improvements in HIV care. Providers can use claims data to refine treatment plans, researchers can analyze patterns in medication effectiveness and long-term outcomes, and policymakers can better allocate resources by identifying areas in need of additional support or intervention. These insights contribute to a more data-driven approach that enhances the quality of HIV care, ensures that treatment remains effective, and supports public health strategies that are aimed at improving outcomes for patients across various different healthcare settings. Through continuous analysis and application, health claims data becomes a powerful tool for making informed decisions that advance both HIV treatment and management.
Using Health Claims Data for Monitoring and Improving Antiviral Treatment
Health claims data is an excellent tool for monitoring patient responses to antiviral medications, that gives healthcare providers the ability to adjust treatment plans based on real-world outcomes. In HIV care, where effective treatment relies on precise medication management, claims data allows providers to track each patient’s adherence to prescribed antivirals and observe their response over time. This continuous monitoring is highly important to help ensure that antiviral therapy properly suppresses the virus, reduces the risk of transmission, and minimizes the chance of drug resistance.
By examining health claims data, healthcare teams can identify patterns in how different patient groups adhere to antiviral regimens and assess which treatments achieve the most consistent viral suppression. For example, if certain demographics or age groups are found to have lower adherence rates, providers can use these insights to develop targeted support, such as adherence counseling or easier-to-manage treatment options. In addition, health claims data allows for the analysis of treatment effectiveness, revealing which antiviral combinations yield the most stable results in maintaining low viral loads.
Health claims data also provides a clear picture of how antiviral prescription practices impact outcomes. By reviewing this data, providers can better evaluate the long-term effectiveness of various medications and refine their prescribing practices accordingly. For instance, if claims data shows that specific antivirals are associated with fewer side effects or better adherence rates in specific populations, healthcare teams can prioritize these medications in their treatment plans. This data-driven approach allows for individualized care, ensuring that patients receive the most suitable medications for their unique health profiles.
In HIV treatment, where patient outcomes can be significantly impacted by small adjustments, health claims data is an invaluable resource for enhancing care quality. By guiding antiviral prescription practices, it helps reduce the risk of HIV-related complications, improves the quality of life for patients, and supports long-term viral suppression. Through careful analysis and application of claims data, healthcare providers can ensure that their approaches to HIV treatment always remain effective, adaptable, and responsive to the needs of different patient populations.
Personalizing HIV Treatment Through Health Claims Data
Health claims data gives healthcare providers the insights they need to customize HIV treatment for individual patients. By analyzing patient profiles, providers can determine which antiviral therapies are most effective for specific demographics or health conditions. For example, claims data might reveal that a particular antiviral combination achieves better outcomes for older patients, while a completely different regimen may be more effective for younger patients.
This data also tracks the long-term efficacy of antiviral combinations and any adjustments to this therapy that may be needed over time. Providers can monitor how well specific regimens control viral loads and identify when a treatment shift is required. For instance, if a patient’s viral suppression declines on a certain medication, claims data can prompt a review, guiding providers toward more effective alternatives. Over time, these adjustments, informed by claims data, lead to optimized patient outcomes by ensuring each individual receives a treatment plan that is specially tailored to their changing needs.
Maximizing Health Claims Data for HIV Research and Policy Development
Health claims data plays a very important role in HIV research by allowing for in-depth studies on treatment effectiveness, demographic trends, and healthcare use patterns. Researchers use this data to track which antiviral therapies are achieving the best results across various patient populations, providing a comprehensive understanding of which treatments lead to better outcomes in real-world settings.
For policymakers, health claims data is invaluable for developing policies that enhance access to antiviral medications and improve HIV care quality. By examining trends in treatment adherence, drug effectiveness, and patient outcomes, policymakers can make informed decisions that address barriers to care and ensure that HIV patients receive access to the resources they need. For example, if claims data indicates that certain populations have low access to effective antivirals, policies can be implemented to address this gap.
Insights from health claims data also guide resource allocation and support public health initiatives that are aimed at HIV prevention and management. By identifying high-need areas or populations, health claims data allows for a much more efficient distribution of resources, ensuring that prevention and treatment efforts reach those most affected by HIV.
Partnering with MDV to Improve HIV Outcomes Through Health Claims Data
Health claims data plays a very important role in HIV care and treatment by providing healthcare providers with essential insights into patient demographics, treatment patterns, and medication adherence. This data is especially valuable in Japan, where comprehensive healthcare datasets allow for a deeper understanding of HIV management and the effectiveness of antiviral therapies. Through health claims data, healthcare teams can refine treatment approaches, ensure continuity of care, and more precisely address individual patient needs.
MDV offers extensive data resources that support advanced analysis and real-world evidence, helping stakeholders make informed decisions that improve HIV care outcomes. The Japanese healthcare system’s emphasis on data accuracy and chronic disease management aligns with MDV’s mission to deliver actionable insights that drive better care practices and support public health initiatives.
For anyone with the goal of enhancing HIV treatment through data-driven solutions, MDV is a valuable partner. We invite healthcare providers, researchers, and policymakers to explore how MDV’s resources can support your goals in HIV care. Contact MDV today to learn more about how our data solutions can lift your approach to patient management and improve health outcomes.
Frequently Asked Questions
How does data analytics impact insurance claims management?
Data analytics enhances insurance claims management by identifying patterns, reducing processing costs, and improving accuracy. Analytics allow insurers to detect trends, streamline workflows, and make more informed decisions, resulting in faster claims processing and better resource allocation.
What is health care claims data?
Health care claims data consists of records submitted by healthcare providers for insurance reimbursement. These records include details on patient diagnoses, treatments, prescribed medications, and healthcare use patterns, offering a complete view of patient care and outcomes.
How can claims data be used in healthcare research?
Claims data allows researchers to analyze treatment patterns, evaluate health outcomes, and support the development of evidence-based healthcare policies. It provides real-world insights that help improve treatment effectiveness and guide healthcare decision-making.
What does claims data tell us about a patient?
Claims data provides a record of a patient’s healthcare history, covering diagnoses, treatments, and medication adherence. This information helps providers understand patient needs, monitor their health progress, and make more informed decisions about their care.
What are the sources of data in insurance companies’ claims?
Insurance claims data is collected from various sources, including hospitals, clinics, outpatient centers, and pharmacies. These sources provide comprehensive healthcare information that insurers use for accurate claims assessment and analysis.analysis and more precise conclusions.
For More Information, Please Contact Us Here
About Japanese Healthcare System

What you need to know about the healthcare system in Japan before using the data.
SERVICE
In addition to various web tools that allow you to easily conduct surveys via a browser using our medical database, we offer data provision services categorized into four types to meet your needs and challenges: "Analysis reports" "Datasets," "All Therapeutic Areas Data Provision Service," and "Specific Therapeutic Areas Data Provision Service.

© Medical Data Vision Co., Ltd. All Rights Reserved.





